Key Takeaways
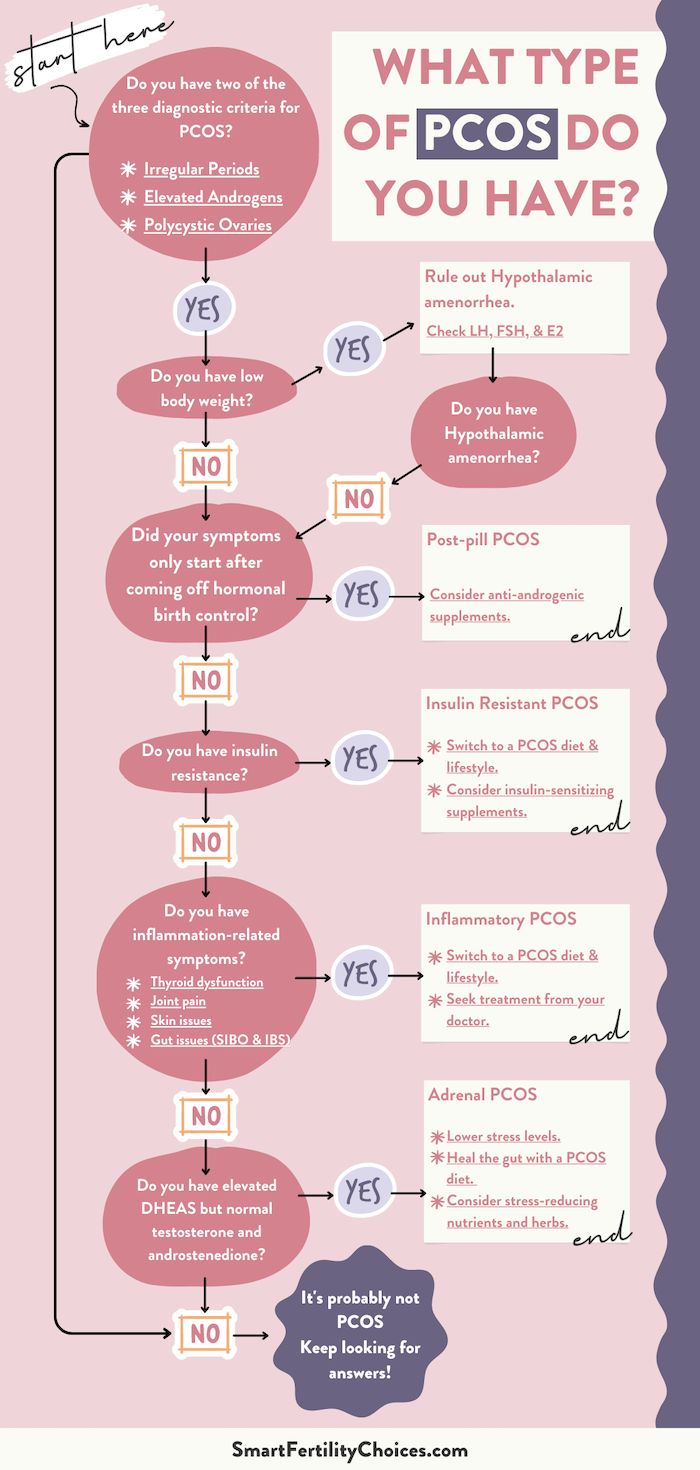
In naturopathic medicine, there are four types of PCOS. Identifying which type you have can help guide your treatment. This article (and the quiz at the end) will walk you through the process.
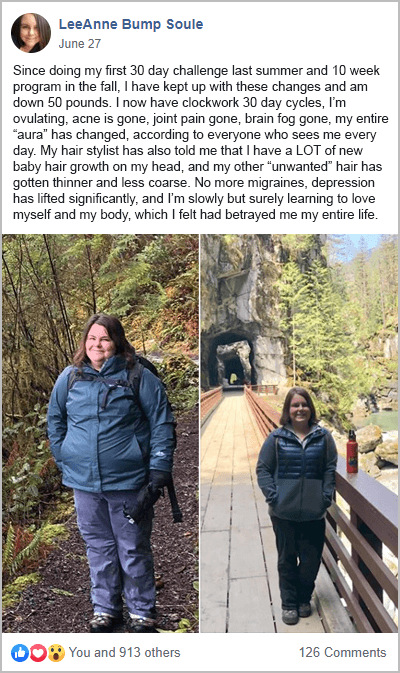
As you’ll discover, a PCOS diet is foundational for health and fertility. This is the case for all types of PCOS. The results from the diverse range of women that complete my free 30-Day PCOS Diet Challenge show this to be true. Download this free 3-Day Meal Plan for a sample of PCOS recipes.
First Check You Meet the Diagnostic Criteria
The first step in identifying which type of PCOS applies to you is checking you actually have PCOS. Polycystic ovarian syndrome comes in all shapes and sizes making it difficult to diagnose. But to have PCOS you must meet at least two of three criteria:
- Irregular periods
- Elevated androgens
- Polycystic ovaries
As you’re about to see, you can meet the diagnostic criteria, and still not have PCOS. But it’s a good place to start.
Summary
You must meet two of three criteria to be diagnosed with PCOS. Irregular periods, elevated androgens, or the presence of polycystic ovaries.
Rule Out Hypothalamic Amenorrhea
The next thing you want to check is that your “PCOS” isn’t hypothalamic amenorrhea (HA). HA looks a lot like lean-type PCOS, but it’s a different diagnosis from polycystic ovary syndrome. If you’re relatively lean, it’s important to rule this diagnosis out.
Hypothalamic amenorrhea is when the control center of your brain causes your periods to stop. It’s typically caused by excessive exercise, stress, and under-eating.
HA is often confused with lean-type PCOS for several reasons. Women with HA can present with polycystic ovaries. They can also have hair loss, excess hair growth, and other signs of mild hirsutism. It’s more likely in women under 30, but it can happen at any age.
The best way to rule out HA is a blood test for luteinizing hormone and follicle-stimulating hormone. PCOS patients have a high LH to FSH ratio (>1). HA patients, by comparison, have a low LH to FSH ratio (<1) [1].
Treatment for HA is mostly focused on eating more and exercising less. Seeing a mental health professional can also be an important part for many people.
Okay. So, you meet the diagnostic criteria, and you’ve ruled out hypothalamic amenorrhea. Now it’s time to consider the four types of PCOS.
Summary
Women with hypothalamic amenorrhea (HA) are often misdiagnosed as having lean-type PCOS. If you have a low body weight, make sure HA has been ruled out.
1. Post-Pill PCOS
When looking at the different types of PCOS, it’s important to consider post-pill PCOS.
Post-pill PCOS is where non-PCOS women show PCOS-like symptoms after going off birth control. Despite the name, this type of PCOS isn’t limited to the oral contraceptive pill. All forms of hormonal birth control can cause post-pill PCOS. This includes the Depo-Provera injection and hormonal IUDs like Mirena and Skyla. Vaginal rings, skin, and subcutaneous patches can also cause post-pill PCOS.
If you didn’t experience PCOS symptoms in the past. And they only began when you stopped taking birth control, then it’s likely you have post-pill PCOS.
The good news about this diagnosis is that it’s generally a temporary problem. It’s not actually a form of polycystic ovary syndrome. Post-pill PCOS can resolve on its own.
Anti-androgenic supplements can also help. Spearmint tea and green tea are effective and safe anti-androgens. Other proven herbs for PCOS include red reishi, licorice, and Chinese peony [2]. Saw palmetto extract is also often used as an anti-androgen.
Summary
Post-pill PCOS is a temporary problem caused by stopping hormonal birth control. This isn’t actually PCOS. But treatment may be similar.
2. Insulin Resistant PCOS
Insulin resistance affects all women with PCOS. Along with poor diet, it’s one of the underlying causes of this syndrome [3, 4]. Even lean PCOS women with normal insulin sensitivity benefit from reducing insulin secretion [5].
But insulin-resistant PCOS is the type of PCOS where insulin resistance is the primary driver of your symptoms. The majority of women with PCOS fit into this category [6, 7]. If you find it particularly difficult to manage your weight, it’s most likely that you have insulin resistance PCOS. But normal-weight women can also have this type of PCOS.
Having a waist-to-hip ratio greater than 0.85 is a simple measure that can indicate insulin resistance in patients with PCOS [8]. But blood testing is the best diagnostic tool.
The best way to treat insulin-resistant PCOS is a lower carbohydrate diet and lifestyle changes. This isn’t just about avoiding high-sugar foods and you don’t need to eat less. Following the best macros for PCOS can sometimes mean eating more. Reducing inflammation can also help you better balance blood sugar levels.
Dietary supplements like inositol, berberine, magnesium, vitamin D, and many others can also be helpful. Learn more about the best PCOS supplements here.
To reverse insulin resistance and improve your health, follow the 15 strategies laid out here. These steps drive weight loss, but they can also help you get pregnant.
Summary
Insulin-resistant PCOS occurs when insulin resistance is the main driver of your symptoms. The best way to treat insulin-resistant PCOS is through diet and lifestyle interventions.
3. Inflammatory PCOS
Like insulin resistance, chronic inflammation is a problem for all types of PCOS. It’s one of the underlying drivers of all PCOS symptoms [9-13].
But inflammatory PCOS is the type of PCOS where inflammation is the primary factor. Many insulin-resistant PCOS patients will share the same symptoms as inflammatory type PCOS. But you only have inflammatory PCOS if you don’t have insulin resistance.
The most obvious indicator of inflammatory PCOS is an autoimmune comorbidity. PCOS is closely associated with autoimmunity as explained more here. This includes thyroid disease and rheumatoid arthritis [14-16]. Skin conditions like sclerosis, psoriasis, and eczema are also common signs of inflammation.
Gut-related issues, especially IBS and SIBO, indicate inflammatory PCOS. These need to be treated with the help of a functional medicine or naturopathic doctor.
Blood testing for C-reactive protein can help identify inflammatory PCOS. This biomarker is high in PCOS women independent of body weight [17].
Women with inflammatory PCOS need to pay particular attention to gut health. Balancing gut bacteria and repairing leaky gut tissue are essential objectives of treatment. This means cutting out all the foods to avoid with PCOS. By addressing potential food sensitivities, you can reduce your inflammatory burden. Cutting out gluten, dairy, sugar, and vegetable oils is the most important place to start. Eating more anti-inflammatory foods, fiber, and vegetables can also make a big difference.
In some cases, a low FODMAP or Autoimmune Protocol diet may be appropriate.
Summary
Inflammatory PCOS occurs when inflammation is the main driver of your symptoms. Treatment should focus on healing the gut. A low-inflammation PCOS diet is essential. But help from a medical professional may also be needed.
4. Adrenal PCOS
Adrenal PCOS should only be suspected once you’ve excluded the other different types of PCOS. It’s caused by exposure to androgen excess in the womb [18, 19]. When coupled with unfavorable environmental factors, this causes an upregulation of the adrenal glands. Too many adrenal androgens are produced resulting in PCOS-like symptoms.
Adrenal PCOS can be identified when DHEA-S levels are the only “male hormone” that’s elevated. You should have normal testosterone and androstenedione levels.
Estimates suggest that high DHEA-S levels affect around 20 – 30% of PCOS patients [20, 21]. But only some of these people will have adrenal PCOS because another type of PCOS will be more dominant.
A naturopathic or functional doctor will treat adrenal PCOS by healing the gut. Diet is critical for balancing gut bacteria and repairing leaky gut tissue. But lowering stress levels is also essential. Many nutritional and herbal products can help support these goals.
Summary
Adrenal PCOS occurs when upregulation of the adrenal glands causes adrenal androgen excess. Treatment should focus on healing the gut with diet and lifestyle changes. Nutritional and herbal supplements for stress can also be helpful.
The Cause of All Types of PCOS
Knowing which type of PCOS you have can help optimize your treatment. But from a patient’s perspective, there’s a simpler way to understand your diagnosis.
All PCOS symptoms are driven by three underlying mechanisms [4, 11-13, 22, 23]:
- Elevated androgens
- Poor insulin regulation
- Chronic inflammation
Each of these factors exists on a spectrum. If your hair falls out or you have acne or hirsutism, then your androgen dial is turned up. If you have trouble maintaining a healthy body weight, then your insulin regulation is likely to be poor. If you don’t get a regular period, then this could be affected by all three mechanisms.
What’s more, none of these factors are static. Major life events can alter your diagnosis. Birth control, pregnancy, and breastfeeding can all alter your physical symptoms. Trauma, surgery, infections, or toxins can also change your immune and endocrine systems.
This simple understanding of PCOS covers all the various ways this diagnosis manifests.
It also points towards the best approach to treatment.
Summary
The same three underlying mechanisms drive all types of PCOS. Androgen excess, poor insulin regulation, and chronic inflammation. The relative impact of each mechanism can change over time. But the root causes remain the same.
Same Foundational Treatment for All PCOS Types
Regardless of which type of PCOS you have, a PCOS-friendly lifestyle provides a foundation for better health.
Imbalances in the gut microbiome drive most of the pathology seen in PCOS [24, 25]. An unhealthy diet is also a primary contributor [3]. Together, poor gut health and a bad diet activate all three mechanisms that drive PCOS.
This is why a PCOS diet is a prerequisite to getting your symptoms under control. If you eat poorly, then any other treatment is likely to have limited benefits. You can see the power of diet change alone from the women that complete my free 30-Day PCOS Diet Challenge. I’ve heard from many women who feel better just after trying my free 3-Day PCOS Meal Plan.

Summary
The right kind of diet treats the underlying factors that drive polycystic ovary syndrome. A PCOS diet is essential for optimizing all other treatments.
Take the Quiz!
The Bottom Line
In naturopathic medicine, there are 4 types of PCOS. Categorizing PCOS into different types helps naturopathic practitioners optimize treatment for their patients.
But from a patient perspective, the best way to understand PCOS is that there are three drivers of all symptoms. Elevated androgens, poor insulin regulation, and chronic inflammation. These factors exist on a spectrum and can change over time.
This is why a PCOS diet is beneficial to everyone. Regardless of your PCOS body type. Start embracing a better diet today with this free 3-Day Meal Plan. Or sign-up here for my free 30-Day PCOS Diet Challenge.
Author
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.
References
1Abou Sherif, S., et al., Investigating the potential of clinical and biochemical markers to differentiate between functional hypothalamic amenorrhoea and polycystic ovarian syndrome: A retrospective observational study. Clin Endocrinol (Oxf), 2021. 95(4): p. 618-627.
2Grant, P. and S. Ramasamy, An update on plant derived anti-androgens. Int J Endocrinol Metab, 2012. 10(2): p. 497-502.
3Barrea, L., et al., Source and amount of carbohydrate in the diet and inflammation in women with polycystic ovary syndrome. Nutr Res Rev, 2018. 31(2): p. 291-301.
4Wang, J., et al., Hyperandrogenemia and insulin resistance: The chief culprit of polycystic ovary syndrome. Life Sciences, 2019. 236.
5Baillargeon, J.P. and A. Carpentier, Role of insulin in the hyperandrogenemia of lean women with polycystic ovary syndrome and normal insulin sensitivity. Fertil Steril, 2007. 88(4): p. 886-93.
6DeUgarte, C.M., A.A. Bartolucci, and R. Azziz, Prevalence of insulin resistance in the polycystic ovary syndrome using the homeostasis model assessment. Fertil Steril, 2005. 83(5): p. 1454-60.
7Legro, R.S., et al., Prevalence and predictors of risk for type 2 diabetes mellitus and impaired glucose tolerance in polycystic ovary syndrome: a prospective, controlled study in 254 affected women. J Clin Endocrinol Metab, 1999. 84(1): p. 165-9.
8Majumdar, A. and T.A. Singh, Comparison of clinical features and health manifestations in lean vs. obese Indian women with polycystic ovarian syndrome. J Hum Reprod Sci, 2009. 2(1): p. 12-7.
9Dimitriadis, G.K., I. Kyrou, and H.S. Randeva, Polycystic Ovary Syndrome as a Proinflammatory State: The Role of Adipokines. Curr Pharm Des, 2016. 22(36): p. 5535-5546.
10Escobar-Morreale, H.F., M. Luque-Ramírez, and F. González, Circulating inflammatory markers in polycystic ovary syndrome: a systematic review and metaanalysis. Fertil Steril, 2011. 95(3): p. 1048-58.e1-2.
11González, F., Inflammation in Polycystic Ovary Syndrome: underpinning of insulin resistance and ovarian dysfunction. Steroids, 2012. 77(4): p. 300-5.
12Popovic, M., G. Sartorius, and M. Christ-Crain, Chronic low-grade inflammation in polycystic ovary syndrome: is there a (patho)-physiological role for interleukin-1? Seminars in Immunopathology, 2019. 41(4): p. 447-459.
13Rudnicka, E., et al., Chronic Low Grade Inflammation in Pathogenesis of PCOS. Int J Mol Sci, 2021. 22(7).
14Garelli, S., et al., High prevalence of chronic thyroiditis in patients with polycystic ovary syndrome. European Journal of Obstetrics & Gynecology and Reproductive Biology, 2013. 169(2): p. 248-251.
15Romitti, M., et al., Association between PCOS and autoimmune thyroid disease: a systematic review and meta-analysis. Endocrine Connections, 2018. 7(11): p. 1158-1167.
16Sharmeen, S., et al., Polycystic ovary syndrome: epidemiologic assessment of prevalence of systemic rheumatic and autoimmune diseases. Clin Rheumatol, 2021. 40(12): p. 4837-4843.
17Aboeldalyl, S., et al., The Role of Chronic Inflammation in Polycystic Ovarian Syndrome-A Systematic Review and Meta-Analysis. Int J Mol Sci, 2021. 22(5).
18Abbott, D.H., et al., Fetal programming of adrenal androgen excess: lessons from a nonhuman primate model of polycystic ovary syndrome. Endocr Dev, 2008. 13: p. 145-158.
19Zhou, R., et al., Adrenal hyperandrogenism is induced by fetal androgen excess in a rhesus monkey model of polycystic ovary syndrome. J Clin Endocrinol Metab, 2005. 90(12): p. 6630-7.
20Yildiz, B.O. and R. Azziz, The adrenal and polycystic ovary syndrome. Rev Endocr Metab Disord, 2007. 8(4): p. 331-42.
21Goodarzi, M.O., E. Carmina, and R. Azziz, DHEA, DHEAS and PCOS. J Steroid Biochem Mol Biol, 2015. 145: p. 213-25.
22Carvalho, L.M.L., et al., Polycystic Ovary Syndrome as a systemic disease with multiple molecular pathways: a narrative review. Endocr Regul, 2018. 52(4): p. 208-221.
23González, F., et al., Hyperandrogenism sensitizes mononuclear cells to promote glucose-induced inflammation in lean reproductive-age women. Am J Physiol Endocrinol Metab, 2012. 302(3): p. E297-306.
24Tremellen, K. and K. Pearce, Dysbiosis of Gut Microbiota (DOGMA)–a novel theory for the development of Polycystic Ovarian Syndrome. Med Hypotheses, 2012. 79(1): p. 104-12.
25Shan, H., et al., Abnormal Endometrial Receptivity and Oxidative Stress in Polycystic Ovary Syndrome. Front Pharmacol, 2022. 13: p. 904942.
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.



