If you’re confused about gluten and polycystic ovarian syndrome, then you’re in good company.
Some people say going gluten-free is good for PCOS. But others say it’s unnecessary at best, and possibly harmful.
What’s the truth?
In my free 30-Day PCOS Diet Challenge I make it pretty clear where I stand on this question. Sure, there’s no direct evidence linking PCOS and gluten. But what we do have, is a lot of indirect information that can inform our decision-making.
In this article I’m going to show you why going gluten-free is a powerful PCOS natural treatment. I’ll also provide information on how to do it successfully.
If you’re ready to cut out gluten already, then you can also download this 3-Day PCOS meal plan.
1. Wheat Allergy, Celiac Disease, & Gluten Sensitivity
Celiac disease is an autoimmune disorder where gluten damages the small intestine. It affects around 1 in 100 people worldwide [1]. Wheat allergy is a gluten-related allergic disorder that affects only 1 in 1000 people [2]. Because wheat allergy and celiac disease are so rare, many experts will claim that for most people, going gluten-free is unnecessary.
Non-celiac gluten sensitivity (NCGS) is a different story though. Also known as gluten sensitivity or gluten intolerance, NCGS may affect as much as 15% of the population [3]. People with gluten sensitivity have a similar problem with gluten as celiac sufferers. The difference though is that they don’t have antibodies that cause intestinal damage [4].
Because of this, gluten sensitivity is hard to diagnose. An intestinal biopsy isn’t helpful and there are no reliable blood tests [5]. It’s also largely glossed over by those that argue that a gluten-free diet can be harmful.
2. The Link Between PCOS & Gluten Sensitivity
In my experience, most women with PCOS have some form of gluten intolerance. This is true whether they’re aware of it or not. This view is informed both by the scientific literature and real-world experience.
The predisposing factors for non-celiac gluten sensitivity are:
- Autoimmune disorders [6, 7]
- Functional gastrointestinal disorders [8-11]
- Being female [12-14]
- Neurological disorders [15-17]
- Eating disorders [17]
- First-degree relatives with celiac disease [12, 17]
- Food allergies and intolerance [17-19]
Through my Beat PCOS 10-Week Program, I’ve had the honor of working with thousands of women with PCOS. Very few of them have not met at least two of these criteria. While still controversial, there’s growing evidence that PCOS is an autoimmune disorder [20, 21].
Autoimmune thyroid disease is also a common comorbidity of PCOS. It affects between 18-40% of women with PCOS. This is approximately three times the rate observed in women without PCOS [22]. A large percentage of these women have what’s known as subclinical hypothyroidism [23]. This means that a diagnosis is easy to miss unless your doctor knows what to look for.
For anyone with PCOS, with any kind of thyroid dysfunction, going gluten-free is especially helpful [24-26].
3. How To Diagnose Gluten Sensitivity
Non-celiac gluten sensitivity can be hard to diagnose. This is because there aren’t any sensitive and specific diagnostics biomarkers [27].
There are many labs and testing companies that offer gluten sensitivity testing. But despite best efforts, these are unreliable.
Celiac disease and wheat allergy must first be excluded. An exclusion diet with a challenge test is then needed. For a formal diagnosis, the challenge test must be double-blinded and placebo-controlled. The Salerno experts’ criteria describe this process [4]. Despite its scientific rigor, there are many practical limitations to this approach [27].
The challenges in diagnosing gluten sensitivity make it hard to prove that gluten is bad for women with PCOS. But from a practical perspective, we can make things much simpler.
As explained above, we know that women with PCOS are at high risk of having some kind of gluten intolerance. But rather than investing in unreliable tests or complicated clinical protocols, we can find the right answer easily.
Go strictly gluten-free for at least a month and see for yourself. You can then do your own challenge test by loading up on gluten-rich foods again. If you have subclinical gluten intolerance, it’s likely to reveal itself to you.
I recommend a similar process for dairy products. See my PCOS and dairy article for more.
4. The Health Benefits Of Going Gluten-Free
As a key aspect of a PCOS diet, going gluten-free can contribute to the following health outcomes:
- Weight loss
- Improved ovulation
- Better gut health
- Improved health skin
- Elimination of brain fog
- Better sleep quality
- Improved emotional regulation
These are big claims, right? Linking a single diet change to a specific health outcome is scientifically challenging. It requires a combination of mechanistic data, epidemiological studies, and randomized controlled trials.
The truth is, we don’t have this kind of data.
What we do have though is a lot of real-life case studies. That isn’t enough to pass rigorous scientific scrutiny but it’s more than enough to see that it works.
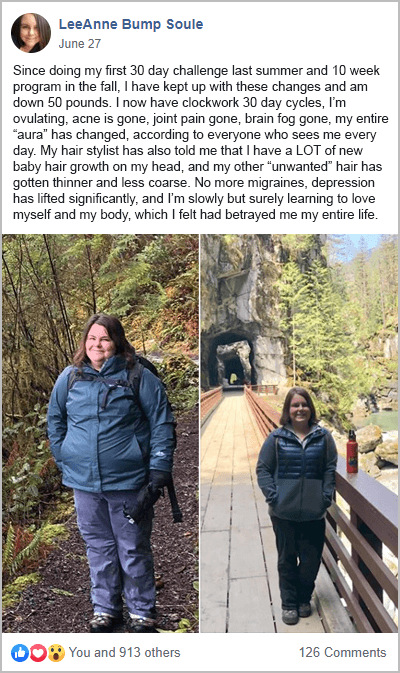
Going gluten-free is a consistent theme in many of my PCOS success stories. Here are a few quotes from my Beat PCOS 10-Week program participants.
“…gluten, in particular, was definitely my worst enemy.” Karina K. Lost 60 lbs and achieved her goal weight.
“What’s changed? I have cut all gluten, dairy, soy, and sugars out of my diet.” Raynetta. Lost 50 lbs and fixed her hirsutism.
“The first thing I noticed when I started eating healthy was that my stomach was no longer swollen after I ate.” Hanna. Fixed her period and fell pregnant naturally.
“I cut out all processed/packaged foods and meats, all gluten, all dairy (except butter), soy, and all high GI carbs.” LeeAnne Soule. Lost 65 lbs and fixed EVERYTHING.
5. How To Go Gluten-Free The Right Way
If you’re ready to go gluten-free to help keep your PCOS in check, then you need to know that there’s a “right way” and a “wrong way” to go about it.
Gluten is a group of proteins found in wheat, rye, and barley. Bread, pasta, pizza, and breakfast cereals are obvious foods to avoid with PCOS. But it’s also found in many processed foods like sauces, dressings, and snacks.
One of the biggest criticisms of a gluten-free diet is that it’s not healthy. Experts have shown that gluten-free processed grain products are often lower in iron, zinc, and potassium [28]. As a result, a gluten-free diet may increase the risk for nutritional deficiencies [29].
Other studies have shown that the consumption of gluten-free foods can increase sugar and reduce fiber intake [30]. This is a particular concern for women that have trouble losing weight with PCOS.
These studies show us that switching out normal foods for gluten-free analogs is not likely to help your cause. What you need instead is a whole-food-based diet that happens to exclude gluten.
A healthy PCOS diet is mostly comprised of healthy fats, protein, and non-starchy vegetables. Starchy vegetables (like sweet potatoes) and gluten-free whole grains need to be consumed in moderation. In combination, these steps reduce inflammation. They also ensure better insulin regulation. Along with hyperandrogenism, inflammation and insulin resistance are the primary drivers of PCOS [31-34]. By addressing these issues, most symptoms can be managed more effectively.
For more information, click here for a list of foods to eat and foods to avoid with PCOS. You can also download this PCOS Diet Cheat Sheet and Foods to Avoid Checklist.
Many women find this free 3-Day Meal Plan is a helpful starting place for going gluten-free with PCOS.
The Bottom Line
Experts are right to say that there’s no direct link between PCOS and gluten. That’s technically true, but it’s missing the point. Most women with PCOS have some kind of gluten intolerance whether they realize it or not.
It makes sense for every woman with PCOS to try a gluten-free diet for at least a month. There are no meaningful risks in doing so, yet the benefits can be life-changing. Rather than spend time and money on diagnostic testing, it’s best to try it and see for yourself. After all, your real-life results are the only thing that matters.
Discover today, how much better you feel without gluten in your diet. Download my free 3-Day Meal Plan and sign-up for my free 30-Day PCOS Diet Challenge.
FAQ
What are the signs and symptoms of gluten sensitivity? Common symptoms of gluten sensitivity include abdominal pain, eczema and/or rash, migraine headaches, “brain fog”, chronic fatigue, diarrhea, depression, anemia, tingling of fingertips, and joint pain.
What are some PCOS-friendly gluten-free grains? Suitable gluten-free grains include quinoa, amaranth, buckwheat, rice, corn, and oats. It’s important when eating these foods to do so in a way that doesn’t cause high blood glucose levels. This is further explained here.
How does gluten affect my PCOS? Gluten increases the permeability of the intestinal lining. This is what’s referred to as “leaky gut” syndrome. Increased gut permeability causes an inflammatory response. Chronic inflammation is one of the underlying causes of PCOS. Through this pathway, gluten consumption can make PCOS symptoms worse.
What do I do if a gluten-free diet doesn’t help? Gluten isn’t the only food that causes symptoms associated with gluten sensitivity. Dairy products can cause similar problems in some people. This is why I recommend a gluten and dairy-free diet for PCOS. The next step, beyond gluten and dairy, is to try a low FODMAP diet.
Author
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.
References
1Singh, P., et al., Global Prevalence of Celiac Disease: Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol, 2018. 16(6): p. 823-836.e2.
2Picarelli, A., et al., Reactivity to dietary gluten: new insights into differential diagnosis among gluten-related gastrointestinal disorders. Pol Arch Med Wewn, 2013. 123(12): p. 708-12.
3Potter, M.D.E., et al., Wheat Intolerance and Chronic Gastrointestinal Symptoms in an Australian Population-based Study: Association Between Wheat Sensitivity, Celiac Disease and Functional Gastrointestinal Disorders. Am J Gastroenterol, 2018. 113(7): p. 1036-1044.
4Catassi, C., et al., Diagnosis of Non-Celiac Gluten Sensitivity (NCGS): The Salerno Experts’ Criteria. Nutrients, 2015. 7(6): p. 4966-77.
5Cárdenas-Torres, F.I., et al., Non-Celiac Gluten Sensitivity: An Update. Medicina (Kaunas), 2021. 57(6).
6Carroccio, A., et al., High Proportions of People With Nonceliac Wheat Sensitivity Have Autoimmune Disease or Antinuclear Antibodies. Gastroenterology, 2015. 149(3): p. 596-603.e1.
7Mansueto, P., et al., Autoimmunity Features in Patients With Non-Celiac Wheat Sensitivity. Am J Gastroenterol, 2021. 116(5): p. 1015-1023.
8Sapone, A., et al., Divergence of gut permeability and mucosal immune gene expression in two gluten-associated conditions: celiac disease and gluten sensitivity. BMC Med, 2011. 9: p. 23.
99Catassi, C., et al., The Overlapping Area of Non-Celiac Gluten Sensitivity (NCGS) and Wheat-Sensitive Irritable Bowel Syndrome (IBS): An Update. Nutrients, 2017. 9(11).
101Shahbazkhani, B., et al., Prevalence of Non-Celiac Gluten Sensitivity in Patients with Refractory Functional Dyspepsia: a Randomized Double-blind Placebo Controlled Trial. Sci Rep, 2020. 10(1): p. 2401.
11Barbaro, M.R., et al., Recent advances in understanding non-celiac gluten sensitivity. F1000Res, 2018. 7.
12Volta, U., et al., An Italian prospective multicenter survey on patients suspected of having non-celiac gluten sensitivity. BMC Med, 2014. 12: p. 85.
13van Gils, T., et al., Prevalence and Characterization of Self-Reported Gluten Sensitivity in The Netherlands. Nutrients, 2016. 8(11).
14Zanini, B., et al., Duodenal histological features in suspected non-celiac gluten sensitivity: new insights into a still undefined condition. Virchows Arch, 2018. 473(2): p. 229-234.
15Hadjivassiliou, M., et al., Neurological Dysfunction in Coeliac Disease and Non-Coeliac Gluten Sensitivity. Am J Gastroenterol, 2016. 111(4): p. 561-7.
16Losurdo, G., et al., Extra-intestinal manifestations of non-celiac gluten sensitivity: An expanding paradigm. World J Gastroenterol, 2018. 24(14): p. 1521-1530.
17Gadelha de Mattos, Y.A., et al., Self-Reported Non-Celiac Gluten Sensitivity in Brazil: Translation, Cultural Adaptation, and Validation of Italian Questionnaire. Nutrients, 2019. 11(4).
18Carroccio, A., et al., Non-celiac wheat sensitivity diagnosed by double-blind placebo-controlled challenge: exploring a new clinical entity. Am J Gastroenterol, 2012. 107(12): p. 1898-906; quiz 1907.
19Carroccio, A., et al., Duodenal and Rectal Mucosa Inflammation in Patients With Non-celiac Wheat Sensitivity. Clin Gastroenterol Hepatol, 2019. 17(4): p. 682-690.e3.
20Mobeen, H., N. Afzal, and M. Kashif, Polycystic Ovary Syndrome May Be an Autoimmune Disorder. Scientifica, 2016.
21Schniewind, H.A., et al., Autoimmunity to the Follicle-Stimulating Hormone Receptor (FSHR) and Luteinizing Hormone Receptor (LHR) in Polycystic Ovarian Syndrome. Int J Mol Sci, 2021. 22(24).
22Romitti, M., et al., Association between PCOS and autoimmune thyroid disease: a systematic review and meta-analysis. Endocrine Connections, 2018. 7(11): p. 1158-1167.
23Garelli, S., et al., High prevalence of chronic thyroiditis in patients with polycystic ovary syndrome. European Journal of Obstetrics & Gynecology and Reproductive Biology, 2013. 169(2): p. 248-251.
24Ihnatowicz, P., et al., The importance of nutritional factors and dietary management of Hashimoto’s thyroiditis. Ann Agric Environ Med, 2020. 27(2): p. 184-193.
25Pobłocki, J., et al., Whether a Gluten-Free Diet Should Be Recommended in Chronic Autoimmune Thyroiditis or Not?-A 12-Month Follow-Up. J Clin Med, 2021. 10(15).
26Krysiak, R., W. Szkróbka, and B. Okopień, The Effect of Gluten-Free Diet on Thyroid Autoimmunity in Drug-Naïve Women with Hashimoto’s Thyroiditis: A Pilot Study. Exp Clin Endocrinol Diabetes, 2019. 127(7): p. 417-422.
27Ierardi, E., et al., Biological markers for non-celiac gluten sensitivity: a question awaiting for a convincing answer. Gastroenterol Hepatol Bed Bench, 2018. 11(3): p. 203-208.
28Missbach, B., et al., Gluten-free food database: the nutritional quality and cost of packaged gluten-free foods. PeerJ, 2015. 3: p. e1337.
29Jones, A.L., The Gluten-Free Diet: Fad or Necessity? Diabetes Spectr, 2017. 30(2): p. 118-123.
30Wild, D., et al., Evidence of high sugar intake, and low fibre and mineral intake, in the gluten-free diet. Aliment Pharmacol Ther, 2010. 32(4): p. 573-81.
31Popovic, M., G. Sartorius, and M. Christ-Crain, Chronic low-grade inflammation in polycystic ovary syndrome: is there a (patho)-physiological role for interleukin-1? Seminars in Immunopathology, 2019. 41(4): p. 447-459.
32González, F., Inflammation in Polycystic Ovary Syndrome: underpinning of insulin resistance and ovarian dysfunction. Steroids, 2012. 77(4): p. 300-5.
33González, F., et al., Hyperandrogenism sensitizes mononuclear cells to promote glucose-induced inflammation in lean reproductive-age women. Am J Physiol Endocrinol Metab, 2012. 302(3): p. E297-306.
34Wang, J., et al., Hyperandrogenemia and insulin resistance: The chief culprit of polycystic ovary syndrome. Life Sciences, 2019. 236.
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.