Key Takeaways
When it comes to managing PCOS with dietary interventions, I have a unique perspective to share with you. That’s because I’m a Nutritionist and I’ve won my own battle with this challenging diagnosis. Using the latest evidence-based information and proven practical tools, my free PCOS food plans have now helped over 100,000 women take back control of their health and fertility.
This free 3-Day PCOS Meal Plan is a great way to get started. But if you’re feeling more adventurous, my free 21-Day PCOS Diet Meal Plan gives you more time to see results.
For a comprehensive diet transformation, join thousands of like-minded women with my free 30-Day PCOS Diet Challenge. Get weekly PCOS meal plans, shopping lists, nutritional video lessons, activities, and more.
As a companion to these free resources, this article describes what a PCOS diet is, how to design your own meal plans, and why it’s important to eat PCOS-friendly.
What is Polycystic Ovary Syndrome (PCOS)?
PCOS is an endocrine disorder that affects roughly 1 in 10 women of childbearing age.
The most common symptoms are irregular menstrual cycles and difficulty with weight loss. Unwanted hair growth, thinning hair, and acne are also commonly caused by high testosterone levels. Your healthcare provider is likely to make several checks before confirming your diagnosis. These include using ultrasound to look for multiple ovarian cysts and blood tests to assess your hormone levels.
How Diet Affects Your PCOS Symptoms
An unhealthy diet is one of the key causes of PCOS [10]. More specifically, imbalances within the gut microbiome can account for all aspects of a PCOS diagnosis [11, 12]. This is true regardless of which type of PCOS you have.
PCOS is driven by two diet-related mechanisms. Inflammation and poor blood sugar regulation. These mechanisms cause the hormonal imbalance that drives the wide range of common PCOS symptoms and health risks [13-18].
If you’ve ever eaten a food that upsets your stomach, you can be sure it’s damaging your intestinal lining. This causes an inflammatory response which then makes all PCOS symptoms worse. Starchy and sugary foods that raise blood sugar levels quickly are also a problem. These readily digested carbohydrate-rich foods result in elevated insulin secretion. When your diet frequently causes high insulin levels, insulin resistance can develop.
Insulin resistance drives weight gain making even modest weight loss exceptionally difficult. It also leads to high blood pressure, high cholesterol levels, and increased heart disease risk. What’s more, insulin resistance exacerbates other PCOS symptoms. This includes challenges with fertility, skin, hair, and mental health. Overweight and obese women are more likely than lean PCOS patients to suffer from insulin resistance.
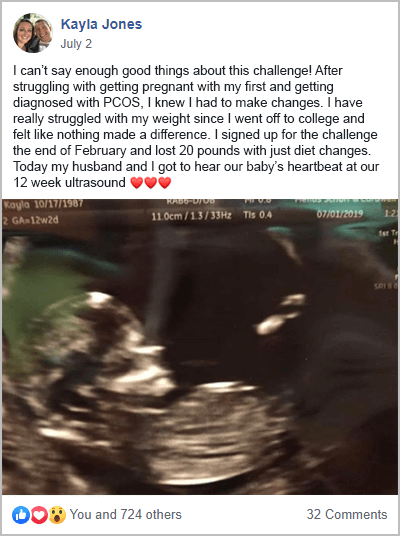
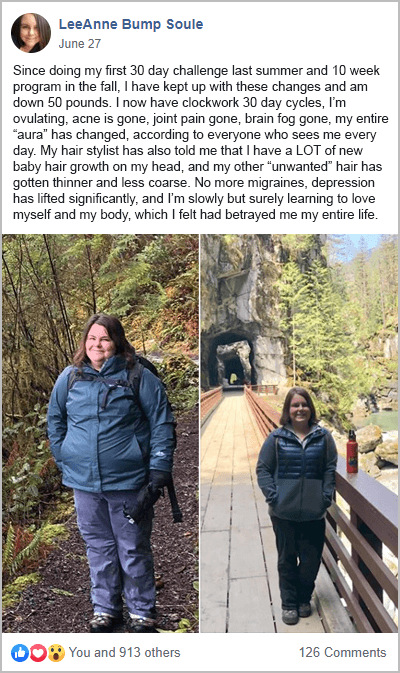
Here are a few women from my free 30-Day PCOS Diet Challenge who learned how powerful a healthy diet can be for managing PCOS symptoms.
Summary
Diet is important for PCOS. It influences the underlying mechanisms that cause poor health and all PCOS symptoms. Diet impacts gut health, inflammation, and insulin regulation. Using a PCOS menu plan can improve PCOS symptoms by addressing these factors.
21-Day PCOS Diet Meal Plan
This free 21-Day PCOS Diet Meal Plan is a great way to get started. You get weekly recipes and shopping lists that you can download in US or metric units. You can also pick your preferred serving size. The 21-Day meal plan eases you into a PCOS diet one week at a time. We tackle breakfast in the first week. Week 2 adds in dinner, while Week 3 is the complete beginner 7-day PCOS diet plan pdf. Unlike most other meal plans creators, I’ve carefully planned each meal for cost and time efficiency. This minimizes meal prep time and any uncooked food going to waste.
3-Day Starter PCOS Diet Plan
If 21 days sounds too overwhelming, I’ve also put together this free 3-Day PCOS Diet Plan pdf. Sample some of my popular, everyday recipes, and get a handy shopping list to make things easy. Anyone can do three days!
PCOS 30-Day Meal Plan Challenge
My free 30-Day PCOS Diet Challenge is what I’m best known for. This isn’t just about providing a great PCOS nutrition plan. Through our online community, you’ll be surrounded by motivated, like-minded people who can help you stay on track. You’ll also receive nutritional video lessons, daily accountability touchpoints, and weekly meal plans and shopping lists.
This program has launched thousands of women toward better overall health and fertility. You can see many of their success stories here.
Breakfast, Lunch, Dinner, Snack, & Dessert Recipes
Just looking for one-off recipes or PCOS meal ideas? Find 37 PCOS recipes to get you started here.
All of these delicious recipes treat PCOS by addressing the two underlying mechanisms. Inflammation and poor blood sugar regulation. With these nutrient-dense recipes, you’ll see for yourself that you can treat PCOS while still enjoying fantastic food. Even my dessert recipes are healthy.
Food to Eat for PCOS
The best foods to eat for PCOS meet at least one of three criteria. They’re good for blood sugar regulation, they promote better gut health, or they reduce inflammation.
The combination of fat, protein, and carbohydrate-rich foods is key for getting blood sugar regulation right. Women with PCOS generally see the best outcomes with a low-carb, high-fat, moderate-protein diet. Getting up to 60% of calories from whole food sources of fat is a powerful way to drive weight loss and reverse insulin resistance. Achieving adequate protein intake also promotes these outcomes [19]. Around 20-30% of energy should come from high-fiber foods that are rich in carbohydrates. High-fiber foods tend to have a low glycemic index (GI) which helps combat insulin resistance. Learn more about a low GI diet and the best macros for PCOS here.
Gut health can be improved with foods high in prebiotic fiber and those containing probiotics. Probiotics are live cultures of “good” gut bacteria. Foods high in prebiotic fiber provide the nutrients they need to thrive.
Non-starchy vegetables should be the largest portion on your plate. Non-starchy vegetables improve gut health and help to reduce insulin resistance. They also provide vitamins, minerals, and unique phytonutrients that make them anti-inflammatory foods.
Here are some of the most PCOS-friendly foods. For a more comprehensive list of nutritious foods to include in your PCOS eating plan, download my PCOS Food List PDF.
Healthy fat-rich foods
- Avocado
- Coconut products
- Eggs
- Nuts and seeds
- Fatty fish (for omega-3 fatty acids)
- Olives and extra virgin olive oil
Healthy carbohydrate-rich foods
- Black, red, wild, and brown rice
- Peas and beans
- Root vegetables
- Sweet potato
- Quinoa
Healthy protein-rich foods
- Meat and eggs
- Fish and seafood
Probiotic foods
- Coconut yogurt
- Natto, Tempeh, and Miso
- Kimchi, sauerkraut and other pickled vegetables
Prebiotic-rich vegetables
- Asparagus
- Artichokes
- Beetroot
- Cabbage
- Fennel bulb
- Garlic
- Onion
- Leek
- Snow peas
Non-starchy vegetables
- Leafy greens, like Romaine lettuce, spinach, and Swiss chard.
- Cruciferous vegetables like bok choy, broccoli, Brussels sprouts, cabbage, cauliflower, and kale.
- Gourd vegetables like cucumber and zucchini.
- Nightshade vegetables like bell peppers, tomatoes, and eggplant.
Summary
Nutrient-dense foods should be balanced for optimum blood sugar regulation. Gut health should be fostered with probiotic and prebiotic-rich foods. Non-starchy vegetables should cover half your plate.
Foods to Avoid for PCOS
There are several key foods to avoid with PCOS. These are all foods that can impact gut health, inflammation, or blood sugar regulation.
Reducing sugar and readily digested carbohydrates improves blood sugar regulation. To minimize inflammation and improve gut health, it’s best to avoid anything that causes noticeable symptoms. This includes things like acid reflux, bloating, abdominal pain, constipation, and diarrhea. For example, many people see noticeable improvements after eliminating gluten from their diet. Learn more about gluten and PCOS here.
PCOS and dairy, also share a fraught relationship as explained here. It’s not just a matter of lactose intolerance. Many people with PCOS have a sensitivity to milk proteins without being aware of it. Like gluten sensitivity, an undiagnosed dairy intolerance can damage the intestinal wall lining. This drives inflammation and worsens the effects of PCOS.
Processed foods, junk food, and fast food are also best avoided. These foods often contain industrial “vegetable” oils, trans fats, and food additives that cause inflammation. This especially applies to fried foods.
The following foods are best avoided or minimized. For a more comprehensive list, download my Foods to Avoid checklist here.
Foods that are bad for blood-sugar regulation
- Anything with a lot of sugar or refined carbohydrates
- Soda and energy drinks
- Cereals
- Cookies, cakes, ice cream
- White bread, brown bread, and bagels
- Pancakes and waffles
- Pasta, white rice, white potatoes
- Chips and pretzels
Foods that drive inflammation
- Any food that’s bad for blood-sugar regulation.
- Gluten, from wheat, spelt, rye, barley, and other whole grains.
- Dairy, including cheeses, yogurt, and protein powders.
- Industrial seed oils from soybeans, sunflower, canola, cottonseed, etc.
- Processed meats such as hot dogs, bacon, sausages, and luncheon meats.
Summary
A good PCOS diet plan excludes foods that negatively affect gut health, inflammation, or blood sugar regulation. Sugar, gluten, dairy, and industrial “vegetable” oils are the most common problem foods. This is why processed foods are discouraged by most PCOS diet experts.
PCOS Diet vs Other Popular Diets
A PCOS diet is a unique approach to nutrition. But it shares nutritional principles with other evidence-based diets.
For example, a PCOS diet is an anti-inflammatory diet. This makes it similar to the Mediterranean diet and the Dietary Approaches to Stop Hypertension (DASH) diet [20]. The key problem with the Mediterranean diet for PCOS is that it includes low-fat dairy and gluten. Otherwise, nourishing foods like whole-grain toast are not helpful for PCOS in my experience.
The problem with the DASH diet is that it unnecessarily restricts saturated fat and salt. Studies show that these restrictions are outdated [21, 22]. Saturated fats from whole food sources shouldn’t be excluded from the “healthy fats” category. This reduces the importance of consuming only lean protein foods like skinless chicken breast. For example, there’s now compelling evidence that beef from well-raised animals can be good for human health and the environment [23, 24].
A PCOS diet is rich in plant foods, like a vegetarian or vegan diet for PCOS. But the problem with plant-only diets is that it’s hard to get adequate protein without consuming too many carbs. This is especially important for weight loss or the treatment of insulin resistance. The same “clean” diet, with the addition of whole food sources of animal protein, is likely to result in better health outcomes.
That’s why I prefer my clients include whole food sources of eggs, fish, and seafood. This makes it well suited to people following a PCOS pescatarian diet. The inclusion of whole food sources of meat also makes my recommendations suitable for people wanting a paleo PCOS meal plan. The only thing that makes my PCOS meals not strictly paleo, is the inclusion of healthy whole grains like rice, corn, quinoa, and buckwheat.
A PCOS diet incorporates the high-fat benefits of a keto diet for PCOS without suffering the downsides of this approach. A PCOS diet is easier to follow than a keto diet. This makes it better suited to people who have experienced disordered eating in the past.
Intermittent fasting can also be included within a PCOS diet framework. Research looking at the effects of fasting specifically on PCOS is limited [25-28]. However many non-PCOS studies show the potential for intermittent fasting to further enhance a PCOS diet [29-31]. Limiting your food intake to 8-12 hours per day is safe for most people [31-35]. This doesn’t mean skipping meals. It just means eating your last meal of the day early or delaying breakfast by a few hours. Even if you find you need to have frequent meals to keep your blood glucose levels stable, this can still be accommodated within a healthy fasting regime.
Unlike many fad diets, a PCOS diet is balanced and sensible. It’s designed to be a sustainable lifestyle intervention.
Summary
A PCOS diet is a unique approach to nutrition. It incorporates the best aspects of other evidence-based diets while avoiding their shortcomings. This includes the Mediterranean diet, the DASH diet, the ketogenic diet, the paleo diet, and more.
Other Ways to Manage PCOS Symptoms
A healthy diet is one of the best interventions for PCOS. But other evidence-based lifestyle changes are well known to further improve health outcomes.
Addressing vitamin deficiencies is an obvious place to start. Especially vitamin D and magnesium. There are many other nutritional supplements for PCOS, with inositol being the most well-proven.
Both aerobic exercise and resistance training can improve PCOS-related hormonal imbalances [36-39].
Studies show that improving sleep quality can reduce food cravings making it easier to eat well [40, 41].
Stress is a known co-morbidity of PCOS [42]. It increases inflammation and can exacerbate insulin resistance [43, 44]. One study found that the most stressed women were twice as likely to suffer from infertility compared to more relaxed women [45].
Summary
Nutritional supplements, exercise, sleep, and other stress management tools enhance the benefits of a PCOS-friendly diet. You’ll achieve your health goals faster by forming better lifestyle habits.
The Bottom Line
Diet is a powerful way to manage PCOS symptoms. That’s because it treats the underlying mechanisms. The right diet can influence gut health, insulin levels, and systemic inflammation.
The most important foods to avoid are gluten, dairy, sugar, “vegetable oils”, and highly processed foods. A PCOS diet is whole-food based and rich in non-starchy vegetables. Macronutrients are balanced to optimize blood sugar regulation.
A good PCOS food plan includes the best aspects of other healthy diets. But it overcomes their shortcomings. The right PCOS nutrition plan can help you lose weight and then maintain a healthy weight long term. It can also help overcome all the other associated symptoms of a PCOS diagnosis. This includes infertility.
Take back control of your health and fertility today by joining my free 30-Day PCOS Diet Challenge. This free 3-Day PCOS Meal Plan is also another great way to get started.
Author
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.
Co-Authors

This blog post has been critically reviewed to ensure accurate interpretation and presentation of the scientific literature by Dr. Jessica A McCoy, Ph.D. Dr McCoy has a master’s degree in cellular and molecular biology, and a doctorate in reproductive biology and environmental health. She currently serves as a University professor at the College of Charleston, South Carolina.

This blog post has also been medically reviewed and approved by Dr. Sarah Lee, M.D. Dr. Lee is a board-certified Physician practicing with Intermountain Healthcare in Utah. She obtained a Bachelor of Science in Biology from the University of Texas at Austin before earning her Doctor of Medicine from UT Health San Antonio.
References
10Barrea, L., et al., Source and amount of carbohydrate in the diet and inflammation in women with polycystic ovary syndrome. Nutr Res Rev, 2018. 31(2): p. 291-301.
11Tremellen, K. and K. Pearce, Dysbiosis of Gut Microbiota (DOGMA)–a novel theory for the development of Polycystic Ovarian Syndrome. Med Hypotheses, 2012. 79(1): p. 104-12.
12He, F.F. and Y.M. Li, Role of gut microbiota in the development of insulin resistance and the mechanism underlying polycystic ovary syndrome: a review. J Ovarian Res, 2020. 13(1): p. 73.
13Carvalho, L.M.L., et al., Polycystic Ovary Syndrome as a systemic disease with multiple molecular pathways: a narrative review. Endocr Regul, 2018. 52(4): p. 208-221.
14González, F., Inflammation in Polycystic Ovary Syndrome: underpinning of insulin resistance and ovarian dysfunction. Steroids, 2012. 77(4): p. 300-5.
15González, F., et al., Hyperandrogenism sensitizes mononuclear cells to promote glucose-induced inflammation in lean reproductive-age women. Am J Physiol Endocrinol Metab, 2012. 302(3): p. E297-306.
16Popovic, M., G. Sartorius, and M. Christ-Crain, Chronic low-grade inflammation in polycystic ovary syndrome: is there a (patho)-physiological role for interleukin-1? Seminars in Immunopathology, 2019. 41(4): p. 447-459.
17Rudnicka, E., et al., Chronic Low Grade Inflammation in Pathogenesis of PCOS. Int J Mol Sci, 2021. 22(7).
18Wang, J., et al., Hyperandrogenemia and insulin resistance: The chief culprit of polycystic ovary syndrome. Life Sciences, 2019. 236.
19Paddon-Jones, D., et al., Protein, weight management, and satiety. Am J Clin Nutr, 2008. 87(5): p. 1558s-1561s.
20Asemi, Z. and A. Esmaillzadeh, DASH diet, insulin resistance, and serum hs-CRP in polycystic ovary syndrome: a randomized controlled clinical trial. Horm Metab Res, 2015. 47(3): p. 232-8.
21O’Donnell, M., et al., Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med, 2014. 371(7): p. 612-23.
22Hite, A.H., et al., In the face of contradictory evidence: report of the Dietary Guidelines for Americans Committee. Nutrition, 2010. 26(10): p. 915-24.
23Provenza, F.D., S.L. Kronberg, and P. Gregorini, Is Grassfed Meat and Dairy Better for Human and Environmental Health? Front Nutr, 2019. 6: p. 26.
24Krusinski, L., et al. Attention to the Details: How Variations in U.S. Grass-Fed Cattle-Feed Supplementation and Finishing Date Influence Human Health. in Frontiers in Sustainable Food Systems. 2022.
25Floyd, R., et al., The Effect of Time-Restricted Eating on Insulin Levels and Insulin Sensitivity in Patients with Polycystic Ovarian Syndrome: A Systematic Review. Int J Endocrinol, 2022. 2022: p. 2830545.
26Chiofalo, B., et al., Fasting as possible complementary approach for polycystic ovary syndrome: Hope or hype? Med Hypotheses, 2017. 105: p. 1-3.
27Han, Y., et al., Time-restricted feeding improves metabolic and endocrine profiles in mice with polycystic ovary syndrome. Front Endocrinol (Lausanne), 2022. 13: p. 1057376.
28Li, C., et al., Eight-hour time-restricted feeding improves endocrine and metabolic profiles in women with anovulatory polycystic ovary syndrome. J Transl Med, 2021. 19(1): p. 148.
29Kang, J., et al., Effect of Time-Restricted Feeding on Anthropometric, Metabolic, and Fitness Parameters: A Systematic Review. J Am Coll Nutr, 2021: p. 1-16.
30Adafer, R., et al., Food Timing, Circadian Rhythm and Chrononutrition: A Systematic Review of Time-Restricted Eating’s Effects on Human Health. Nutrients, 2020. 12(12).
31Moon, S., et al., Beneficial Effects of Time-Restricted Eating on Metabolic Diseases: A Systemic Review and Meta-Analysis. Nutrients, 2020. 12(5).
32Gabel, K., et al., Time-Restricted Eating to Improve Cardiovascular Health. Curr Atheroscler Rep, 2021. 23(5): p. 22.
33Moro, T., et al., Twelve Months of Time-restricted Eating and Resistance Training Improves Inflammatory Markers and Cardiometabolic Risk Factors. Med Sci Sports Exerc, 2021. 53(12): p. 2577-2585.
34Uldal, S., et al., Is Time-Restricted Eating Safe in the Treatment of Type 2 Diabetes?-A Review of Intervention Studies. Nutrients, 2022. 14(11).
35Anic, K., et al., Intermittent Fasting-Short- and Long-Term Quality of Life, Fatigue, and Safety in Healthy Volunteers: A Prospective, Clinical Trial. Nutrients, 2022. 14(19).
36Almenning, I., et al., Effects of High Intensity Interval Training and Strength Training on Metabolic, Cardiovascular and Hormonal Outcomes in Women with Polycystic Ovary Syndrome: A Pilot Study. PLoS One, 2015. 10(9): p. e0138793.
37Cheema, B.S., L. Vizza, and S. Swaraj, Progressive resistance training in polycystic ovary syndrome: can pumping iron improve clinical outcomes? Sports Med, 2014. 44(9): p. 1197-207.
38Covington, J.D., et al., Higher circulating leukocytes in women with PCOS is reversed by aerobic exercise. Biochimie, 2016. 124: p. 27-33.
39Kogure, G.S., et al., Resistance Exercise Impacts Lean Muscle Mass in Women with Polycystic Ovary Syndrome. Med Sci Sports Exerc, 2016. 48(4): p. 589-98.
40Blumfield, M.L., et al., Dietary disinhibition mediates the relationship between poor sleep quality and body weight. Appetite, 2018. 120: p. 602-608.
41Al Khatib, H.K., et al., Sleep extension is a feasible lifestyle intervention in free-living adults who are habitually short sleepers: a potential strategy for decreasing intake of free sugars? A randomized controlled pilot study. Am J Clin Nutr, 2018. 107(1): p. 43-53.
42Benson, S., et al., Disturbed stress responses in women with polycystic ovary syndrome. Psychoneuroendocrinology, 2009. 34(5): p. 727-35.
43Hackett, R.A. and A. Steptoe, Type 2 diabetes mellitus and psychological stress – a modifiable risk factor. Nat Rev Endocrinol, 2017. 13(9): p. 547-560.
44Wirtz, P.H. and R. von Känel, Psychological Stress, Inflammation, and Coronary Heart Disease. Curr Cardiol Rep, 2017. 19(11): p. 111.
45Lynch, C.D., et al., Preconception stress increases the risk of infertility: results from a couple-based prospective cohort study–the LIFE study. Hum Reprod, 2014. 29(5): p. 1067-75.
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.
Co-Authors

This blog post has been critically reviewed to ensure accurate interpretation and presentation of the scientific literature by Dr. Jessica A McCoy, Ph.D. Dr McCoy has a master’s degree in cellular and molecular biology, and a doctorate in reproductive biology and environmental health. She currently serves as a University professor at the College of Charleston, South Carolina.

This blog post has also been medically reviewed and approved by Dr. Sarah Lee, M.D. Dr. Lee is a board-certified Physician practicing with Intermountain Healthcare in Utah. She obtained a Bachelor of Science in Biology from the University of Texas at Austin before earning her Doctor of Medicine from UT Health San Antonio.