A lot of women with PCOS have inadequate levels of magnesium. This is an avoidable cost to your health and fertility.
This article tells you everything you need to know about magnesium for PCOS. You’ll discover the benefits, tips on blood testing, and how to supplement this essential nutrient.
Magnesium supplements make a lot of sense for women with PCOS. But following a PCOS diet like the one we use during my free 30-Day PCOS Diet Challenge is the best way to increase your magnesium intake. This also treats the underlying causes of all PCOS symptoms.
How Much is Enough Magnesium
Women are supposed to get 9.6 mg of dietary magnesium per pound of body weight each day [1]. Most of us aren’t getting there [2]. According to RDA calculations, that’s around 450 – 530 mg/day for the average woman. This is a lot higher than the current recommended daily allowances which experts argue need to be revised [1].
Inadequate dietary intake of magnesium is society-wide. The United States NHANES 2005–2006 survey reported that nearly half of American adults have an inadequate intake. More recent estimates put this figure at 60% [3].
For women with PCOS, the problem is even worse [4].
Why PCOS Women Have Low Magnesium
Women with PCOS are more likely to have low levels of many important minerals including magnesium [5, 6].
Several PCOS-related risk factors account for this finding.
- Being overweight [7].
- Insulin resistance [8-11].
- Medications like metformin and birth control [12, 13].
Magnesium plays a key role in health and disease prevention [2, 14]. Because magnesium is a cofactor in over 300 enzyme systems, inadequate levels can contribute to a range of PCOS symptoms.
Benefits of Magnesium for PCOS
There are three underlying drivers of all PCOS symptoms. Insulin resistance, elevated androgens, and chronic inflammation [15-20]. Magnesium can act on all three of these mechanisms [8, 9, 21-24]. This is why it has a significant effect on PCOS hormone imbalances [25]. The net effect is that magnesium supplements can impact a wide range of symptoms.
- Magnesium may help with PCOS weight loss [25].
- When combined with vitamin E, zinc, and calcium, magnesium can improve metabolic dysfunction in women with PCOS [23, 26].
- Magnesium supplementation on its own can lower blood pressure [27, 28].
- When coupled with vitamin E, modest doses can reduce measures of hirsutism [29]. This is because magnesium and vitamin E have antioxidant and anti-inflammatory properties.
- Magnesium supplements can help prevent premenstrual syndrome, painful periods, and menstrual migraines [5].
- Magnesium has been shown to improve a range of metrics relating to quality of life among women with PCOS. This includes things like energy/fatigue, social functioning, and emotional well-being [30]. It can also help with mild anxiety [31, 32].
Best Foods for Magnesium
A nutrient-dense PCOS diet is the best way to up your magnesium intake. This is because a PCOS diet includes a lot of magnesium-rich foods. Pumpkin seeds, chia seeds, and almonds are some of the richest sources of dietary magnesium. But leafy greens like Swiss chard, spinach, basil, and kale are also high in magnesium.
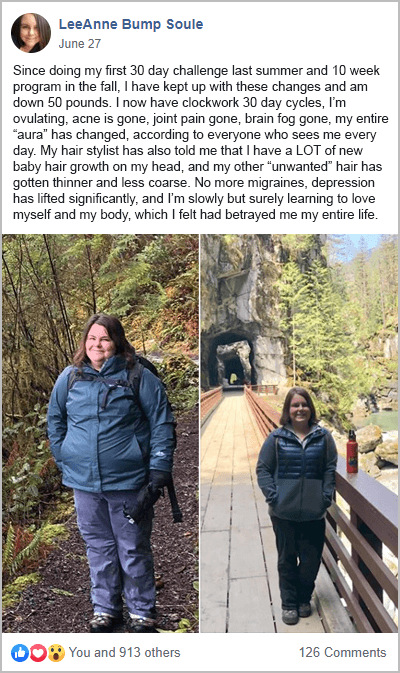
I use many of these ingredients in my PCOS recipes. This includes those in my free 30-Day PCOS Diet Challenge and free 3-Day PCOS meal plan. The addition of magnesium-rich foods, may in part, account for the great results women see when they make the right changes to their diet.

What Type of Magnesium for PCOS
There are several different types of magnesium supplements, each with different benefits.
- Magnesium oxide is poorly absorbed and is mostly used for heartburn and constipation.
- Magnesium citrate is often used as a laxative too, but it’s better absorbed than magnesium oxide.
- Magnesium glycinate is often used to support sleep, and relaxation, and for general supplementation.
- Magnesium bisglycinate is a newer form of magnesium glycinate. It has higher absorption rates and may be better for people with digestive concerns.
- Magnesium threonate may be the best type of magnesium for improving brain and memory function.
- Magnesium malate supports energy production and reduces pain and fatigue.
In general, the best magnesium products for PCOS use either bisglycinate, threonate, or malate forms.
Recommended Magnesium Products
Magnesium supplementation alone doesn’t provide much benefit [23]. Research shows that when supplementing magnesium, you also want to take vitamins D and E, zinc, and calcium [25, 29].
That’s why I recommend Women’s Multi 50+ by Thorne Research. This product includes 180 mg of magnesium malate and ticks all the boxes concerning other essential nutrients. Another thing that sets it apart is the exclusion of copper and iron. Both of these nutrients are known to be higher in women with PCOS compared to healthy controls [33]. Multi-vitamins that contain copper and iron are probably a bad idea for PCOS women.
But what if you’re already taking a good multivitamin and only want a pure magnesium supplement? In this instance, then I recommend Thorne’s magnesium bisglycinate powder.
Thorne Research is a well-respected supplement brand. As I explain in my article on Berberine for PCOS, they have many third-party certifications.
How to Test Magnesium Levels
To optimize magnesium levels, blood testing is needed. Being an informed patient is essential during this process.
Serum magnesium is the most common blood test for assessing magnesium levels. But many physicians fail to understand its limitations [34]. Only 1 % of magnesium is found in serum. Most of it is found in bones, muscles, and other soft tissues. Because of this, reference ranges need updating. A reference range of 0.7 to 1.0 mmol/L is considered normal. That’s the same as 1.7 to 2.4 mg/dL. Yet studies show that values less than 0.85 mmol/L (2.1 mg/dL) are associated with increased health risks [35].
For decades, it’s been known that a “normal” serum magnesium test result doesn’t indicate optimal magnesium status. You really want to be at the upper end of normal ranges [3, 35, 36].
Safety & Side Effects of Magnesium Supplements
Too much magnesium from food isn’t a problem. Adverse effects from supplementation are also limited because the body will only absorb as much as it needs.
The most likely issue with too much magnesium is GI distress and diarrhea. The less bioavailable forms of magnesium are more likely to have this effect which is why they’re used as laxatives.
Most experts agree that doses of 350 mg per day are safe for most adults.
Magnesium supplements can also interact with some medications. For women with PCOS, it’s important to be aware of interactions with levothyroxine and some Type 2 diabetes medications.
Antibiotics, and blood pressure medications can also interact with some magnesium supplements.
When taking doses higher than those used in products like Women’s Multi 50+, it pays to check in with your doctor first.
The Bottom Line
Women with PCOS have a high risk of insufficient magnesium levels. Part of this is due to PCOS-related factors, but inadequate dietary intake is a widespread problem. Increased intake either through diet or supplementation can help manage many PCOS symptoms. Most notably, increased magnesium intake may help with weight loss and metabolic dysfunction. It can also help with hirsutism, menstrual problems, and emotional well-being.
Standard blood testing for magnesium is inaccurate. So it’s important to understand what acceptable levels should be.
The best way to up your magnesium levels is by following a PCOS diet. You can get started today with my free 3-Day Meal Plan and free 30-Day PCOS Diet Challenge.
When considering magnesium supplements, a multivitamin product is best. But caution is warranted when taking higher doses of magnesium along with other medications.
Author
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.
References
1Rosanoff, A., Perspective: US Adult Magnesium Requirements Need Updating: Impacts of Rising Body Weights and Data-Derived Variance. Adv Nutr, 2021. 12(2): p. 298-304.
2Gröber, U., J. Schmidt, and K. Kisters, Magnesium in Prevention and Therapy. Nutrients, 2015. 7(9): p. 8199-226.
3Workinger, J.L., R.P. Doyle, and J. Bortz, Challenges in the Diagnosis of Magnesium Status. Nutrients, 2018. 10(9).
4Kazemi, M., et al., Comparison of dietary and physical activity behaviors in women with and without polycystic ovary syndrome: a systematic review and meta-analysis of 39471 women. Hum Reprod Update, 2022. 28(6): p. 910-955.
5Parazzini, F., M. Di Martino, and P. Pellegrino, Magnesium in the gynecological practice: a literature review. Magnes Res, 2017. 30(1): p. 1-7.
6Szczuko, M., et al., Quantitative assessment of nutrition in patients with polycystic ovary syndrome (PCOS). Rocz Panstw Zakl Hig, 2016. 67(4): p. 419-426.
7Babapour, M., et al., Associations Between Serum Magnesium Concentrations and Polycystic Ovary Syndrome Status: a Systematic Review and Meta-analysis. Biol Trace Elem Res, 2021. 199(4): p. 1297-1305.
8Chakraborty, P., et al., Altered trace mineral milieu might play an aetiological role in the pathogenesis of polycystic ovary syndrome. Biol Trace Elem Res, 2013. 152(1): p. 9-15.
9Hamilton, K.P., et al., Insulin Resistance and Serum Magnesium Concentrations among Women with Polycystic Ovary Syndrome. Curr Dev Nutr, 2019. 3(11): p. nzz108.
10Sharifi, F., et al., Serum magnesium concentrations in polycystic ovary syndrome and its association with insulin resistance. Gynecol Endocrinol, 2012. 28(1): p. 7-11.
11Xu, L.H. and N.M. Maalouf, Effect of acute hyperinsulinemia on magnesium homeostasis in humans. Diabetes Metab Res Rev, 2017. 33(2).
12Wakeman, M. and D.T. Archer, Metformin and Micronutrient Status in Type 2 Diabetes: Does Polypharmacy Involving Acid-Suppressing Medications Affect Vitamin B12 Levels? Diabetes Metab Syndr Obes, 2020. 13: p. 2093-2108.
13Palmery, M., et al., Oral contraceptives and changes in nutritional requirements. Eur Rev Med Pharmacol Sci, 2013. 17(13): p. 1804-13.
14Schwalfenberg, G.K. and S.J. Genuis, The Importance of Magnesium in Clinical Healthcare. Scientifica (Cairo), 2017. 2017: p. 4179326.
15Carvalho, L.M.L., et al., Polycystic Ovary Syndrome as a systemic disease with multiple molecular pathways: a narrative review. Endocr Regul, 2018. 52(4): p. 208-221.
16González, F., Inflammation in Polycystic Ovary Syndrome: underpinning of insulin resistance and ovarian dysfunction. Steroids, 2012. 77(4): p. 300-5.
17González, F., et al., Hyperandrogenism sensitizes mononuclear cells to promote glucose-induced inflammation in lean reproductive-age women. Am J Physiol Endocrinol Metab, 2012. 302(3): p. E297-306.
18Popovic, M., G. Sartorius, and M. Christ-Crain, Chronic low-grade inflammation in polycystic ovary syndrome: is there a (patho)-physiological role for interleukin-1? Seminars in Immunopathology, 2019. 41(4): p. 447-459.
19Rudnicka, E., et al., Chronic Low Grade Inflammation in Pathogenesis of PCOS. Int J Mol Sci, 2021. 22(7).
20Wang, J., et al., Hyperandrogenemia and insulin resistance: The chief culprit of polycystic ovary syndrome. Life Sciences, 2019. 236.
21Afshar Ebrahimi, F., et al., The Effects of Magnesium and Zinc Co-Supplementation on Biomarkers of Inflammation and Oxidative Stress, and Gene Expression Related to Inflammation in Polycystic Ovary Syndrome: a Randomized Controlled Clinical Trial. Biol Trace Elem Res, 2018. 184(2): p. 300-307.
22Cutler, D.A., S.M. Pride, and A.P. Cheung, Low intakes of dietary fiber and magnesium are associated with insulin resistance and hyperandrogenism in polycystic ovary syndrome: A cohort study. Food Sci Nutr, 2019. 7(4): p. 1426-1437.
23Li, R., et al., The effect of magnesium alone or its combination with other supplements on the markers of inflammation, OS and metabolism in women with polycystic ovarian syndrome (PCOS): A systematic review. Front Endocrinol (Lausanne), 2022. 13: p. 974042.
24Luo, X., et al., Associations of Serum Magnesium With Insulin Resistance and Testosterone in Women With Polycystic Ovary Syndrome. Front Endocrinol (Lausanne), 2021. 12: p. 683040.
25Farsinejad-Marj, M., et al., Clinical and Metabolic Responses to Magnesium Supplementation in Women with Polycystic Ovary Syndrome. Biol Trace Elem Res, 2020. 196(2): p. 349-358.
26Jamilian, M., N.K. Sabzevar, and Z. Asemi, The Effect of Magnesium and Vitamin E Co-Supplementation on Glycemic Control and Markers of Cardio-Metabolic Risk in Women with Polycystic Ovary Syndrome: A Randomized, Double-Blind, Placebo-Controlled Trial. Horm Metab Res, 2019. 51(2): p. 100-105.
27Asbaghi, O., et al., The Effects of Magnesium Supplementation on Blood Pressure and Obesity Measure Among Type 2 Diabetes Patient: a Systematic Review and Meta-analysis of Randomized Controlled Trials. Biol Trace Elem Res, 2021. 199(2): p. 413-424.
28Zhang, X., et al., Effects of Magnesium Supplementation on Blood Pressure: A Meta-Analysis of Randomized Double-Blind Placebo-Controlled Trials. Hypertension, 2016. 68(2): p. 324-33.
29Shokrpour, M. and Z. Asemi, The Effects of Magnesium and Vitamin E Co-Supplementation on Hormonal Status and Biomarkers of Inflammation and Oxidative Stress in Women with Polycystic Ovary Syndrome. Biol Trace Elem Res, 2019. 191(1): p. 54-60.
30Jaripur, M., et al., The effects of magnesium supplementation on abnormal uterine bleeding, alopecia, quality of life, and acne in women with polycystic ovary syndrome: a randomized clinical trial. Reprod Biol Endocrinol, 2022. 20(1): p. 110.
31Boyle, N.B., C. Lawton, and L. Dye, The Effects of Magnesium Supplementation on Subjective Anxiety and Stress-A Systematic Review. Nutrients, 2017. 9(5).
32Boyle, N.B., C.L. Lawton, and L. Dye, The effects of magnesium supplementation on subjective anxiety. Magnes Res, 2016. 29(3): p. 120-125.
33Yin, J., et al., Serum Trace Elements in Patients With Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne), 2020. 11: p. 572384.
34Costello, R.B. and F. Nielsen, Interpreting magnesium status to enhance clinical care: key indicators. Curr Opin Clin Nutr Metab Care, 2017. 20(6): p. 504-511.
35Micke, O., et al., Serum magnesium: time for a standardized and evidence-based reference range. Magnes Res, 2021. 34(2): p. 84-89.
36Ismail, Y., A.A. Ismail, and A.A. Ismail, The underestimated problem of using serum magnesium measurements to exclude magnesium deficiency in adults; a health warning is needed for “normal” results. Clin Chem Lab Med, 2010. 48(3): p. 323-7.
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.



