The ketogenic diet is popular among women with polycystic ovary syndrome (PCOS). But, if you’re not careful, it can cause more harm than good.
PCOS is driven by high carbohydrate intake, low-grade inflammation, insulin resistance, and elevated androgen levels [1]. The ketogenic diet can treat PCOS by removing almost all dietary carbohydrates.
But effective doesn’t mean safe or optimal. Other alternatives, like the diet we use in my free 30-Day PCOS Diet Challenge, may be more suitable. Download this free 3-Day Meal Plan for a sample of PCOS-friendly recipes.
This article will help you decide if the keto diet is right for you.
1. Pro: Improves Insulin Resistance
Best estimates suggest insulin resistance affects between 30 and 70% of women with PCOS [2, 3]. The severity of insulin resistance largely determines the strength of PCOS symptoms. Overweight and obese women are more likely to be insulin resistant. But it affects all types of PCOS.
Insulin resistance is a known risk factor for type 2 diabetes, liver disease, heart attack, and stroke. In women with PCOS, insulin resistance contributes to menstrual irregularities and infertility [4]. Studies also show that insulin is associated with depression [5].
A ketogenic diet is a very low carbohydrate diet. It improves PCOS by reversing the effects of insulin resistance. Carb intake needs to be so low, that there isn’t enough glucose to meet the body’s energy requirements. The body then switches to burning fat by-products (ketones) instead of glucose. This lowers insulin levels and the negative effects of insulin resistance [6, 7].
Ketosis can be a powerful way to reduce body fat. For overweight women with PCOS, this can help with weight loss, irregular periods, unwanted body hair, high blood pressure, and more.
Summary
A ketogenic diet can reduce insulin resistance in women with PCOS. This can help you lose weight, improve your menstrual cycle, and reduce other PCOS symptoms.
2. Pro: Sex Hormones, Metabolic Health, & Body Composition
Within the scientific community, the benefits of a keto diet for PCOS are unclear. The size, duration, or other confounding factors limit the clinical significance of the findings. Despite these constraints, there are still several pilot studies that show positive results.
- Mavropoulos et al. 2005 [8] studied 5 women over 6 months. They saw both weight loss and improvements in sex hormone imbalances.
- Paoli et al. 2020 [9] studied 14 women over 12 weeks. They observed improvements in body composition and insulin regulation. Luteinizing hormone, testosterone, and DHEA levels were reduced. Triglyceride and cholesterol levels also improved. This study restricted caloric intake to 1600 kcal per day.
- Cincione et al. 2021 [10] studied 17 women over 45 days. They observed improvements in luteinizing hormone and follicle-stimulating hormone. They also saw better sex hormone binding globulin levels and improved insulin sensitivity. Patients lost 12.4 lb (5.6 kg) on average and showed other improvements in markers of body composition (waist and hip circumference, etc.). It should be noted that this study also restricted caloric intake to just 600 kcal per day. A low caloric intake by any measure. This last point is often missed by people referencing the Cincione et al. study.
The PCOS participants in these studies were between the ages of 18 and 45. They had a body mass index (BMI) > 25 kg/m2 which is within the overweight range. They were not pregnant or breastfeeding, and they had no other serious medical conditions.
When looking at ketogenic diet studies, it’s important to look at the characteristics of the participants. This can have a significant impact on the applicability of the results. Sex, body weight, age, and health status all impact the risks and benefits of very low carbohydrate diets. You need to keep this in mind when assessing the pros and cons.
For example, some experts are open to using a well-formulated ketogenic diet as a first-line treatment for obesity and diabetes [11]. A ketogenic Mediterranean diet, for example, is popular among healthcare professionals. Learn more about the pros and cons of the Mediterranean diet for PCOS here. For women with PCOS more generally though, others urge greater caution.
According to Dr. Jennifer T. Batch M.D and colleagues, the benefits of a ketogenic diet are generally not seen beyond 12 months. The impact on fertility is unclear, and the long-term implications are not well-understood. For example, Batch points out that the diet has a favorable effect on HDL-cholesterol levels. But increases in very low-density LDL may increase cardiovascular risks [6].
Summary
There’s insufficient evidence to support the use of a ketogenic diet as a long-term PCOS treatment. Most trials to date are short-term. They use significant caloric restriction and only include overweight and obese patients.
3. Con: It’s Not Tailored For Polycystic Ovarian Syndrome
Given that the only rule of a ketogenic diet is to reach nutritional ketosis, it’s easy to see the shortcomings in this approach. A diet that’s designed with PCOS in mind is likely to be more suitable.
For example, a ketogenic diet provides no guidance on the suitability of gluten or dairy beyond their impact on ketosis. It’s common for women with PCOS to have a subclinical intolerance to gluten and dairy proteins. This means that these ingredients are generally best avoided. When left undiagnosed, gluten or dairy sensitivity can undermine the intestinal wall lining. This causes inflammation [12]. Low-grade chronic inflammation is a key mechanism in the pathology of PCOS. Because of this, including gluten and dairy in a ketogenic diet can be counter-productive.
Sometimes referred to as “junk keto”, processed, and pro-inflammatory foods are also allowed on a keto diet. Vegetable oils, processed foods, soy, and artificial sweeteners are acceptable. Yet, these are all foods to avoid with PCOS.
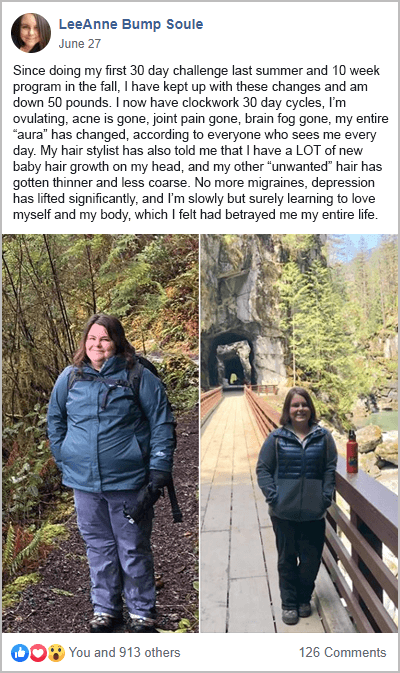
In isolation, each dietary change has a small effect. But a holistic PCOS diet can lead to life-changing results. This is what my free 30-Day PCOS Diet Challenge is all about. The results speak for themselves.
Summary
A ketogenic diet is not suitable for PCOS because it doesn’t restrict gluten, dairy, or other important foods to avoid.
4. Con: May Cause Nutrient Deficiencies
One of the least disputed drawbacks of the ketogenic diet is its lack of nutritional balance.
The ketogenic diet is nutritionally imbalanced. It has the potential to cause vitamin and mineral deficiencies. These include calcium, phosphorus, magnesium, and selenium [13, 14].
The study by Cincione et al. 2021, cited above, issued multivitamin and multimineral supplements to avoid this very problem.
Women with PCOS already have elevated risks for various deficiencies. Magnesium and vitamin D are two stand-outs. Common medications taken by PCOS patients also cause nutrient depletions. Examples include hormonal birth control and Metformin.
Learn more about the best PCOS supplements here.
Summary
Without nutritional supplementation, a ketogenic diet can lead to nutrient deficiencies.
5. Con: It’s Hard On Gut Health
Another key problem with the ketogenic diet is its effects on the gut microbiome. It’s common for people following a keto diet to consume inadequate amounts of fermentable, prebiotic fibers. This includes things like pectin, inulin, and oligofructose. This is because we usually get these important nutrients from fruits, starchy vegetables, and legumes. But with a ketogenic diet, these foods all need to be restricted because of their carbohydrate content.
Experienced clinicians have observed gut dysbiosis in patients following a ketogenic diet. They speculate that this could open the door for pathogens to colonize the gut. Recent evidence has also linked a diet low in fermentable fibers to inflammatory diseases like PCOS [15].
Summary
The ketogenic diet can adversely affect the gut microbiome. This may make PCOS symptoms worse.
6. Con: Can Be Psychologically Unhealthy
Leaving health and fertility aside, maintaining nutritional ketosis can be psychologically difficult. Disordered eating affects women with PCOS roughly five times as much as the general population. Eating disorders are especially likely if they also suffer from anxiety or depression [16]. Severe carbohydrate restriction is necessary to maintain nutritional ketosis For many people, this demand may further deteriorate an already tenuous relationship with food.
Summary
The ketogenic diet can induce disordered eating in at-risk PCOS patients.
7. Con: Harder To Follow For PCOS Women
PCOS may also make it harder to follow a ketogenic diet.
PCOS is characterized by hormone dysregulation. These imbalances are associated with increased appetite, impaired impulse control, and feelings of body dissatisfaction. That’s why there’s so much overlap between PCOS and binge eating [17]. Through this pathway, the hormone dysregulation caused by PCOS can undermine a ketogenic diet. Because even modest over-consumption of carbohydrates can break ketosis.
Summary
The hormone dysregulation that characterizes PCOS makes it more difficult to follow a ketogenic diet.
8. Con: Ketosis Can Make PCOS Worse
Evidence suggests that the keto diet may be beneficial in the short term. But a ketogenic diet may make PCOS worse over the long term:
- 45% of adolescent females reported menstrual dysfunction after following a ketogenic diet [18]. Menstrual dysfunction is a known side-effect of ketosis.
- Overly restricting carbohydrate consumption may negatively impact thyroid function [19]. Given the high prevalence of thyroid dysfunction in the PCOS population [20], this presents an added risk.
- A keto diet is typically short-term, whether by design or as a consequence of how hard it is to stay in ketosis. This feeds into the cycle of yo-yo dieting which is both emotionally and metabolically unhealthy. If like traditional restriction diets, a ketogenic diet results in weight gain over the long term, then it can make your PCOS problems worse.
Summary
Nutritional ketosis can dysregulate hormones and may impact thyroid function.
9. Con: There Are Better Diets For PCOS
The best opposing argument against a ketogenic diet for PCOS is that there’s a much better alternative.
A PCOS diet offers the same freedom from caloric restriction, while also achieving better outcomes.
Unlike the ketogenic diet, which only targets insulin, a PCOS diet also reduces inflammation. This is achieved by avoiding problematic foods and replacing them with better alternatives.
A PCOS diet is low carb, but not very low carb like the ketogenic diet. See my article on macros for PCOS here. I recommend women get around 20-30% of their energy from low-GI carbohydrate foods. This allows for much greater dietary flexibility while still addressing insulin resistance. Intermittent fasting can further enhance these benefits. As a result, a PCOS diet can include many more important and fun foods. Occasional deviations also have little-to-no significant impact on progress.
Unlike a ketogenic diet, a PCOS diet is a long-term lifestyle intervention. Because it doesn’t “feel like a diet”, this treatment safely and effectively manages PCOS symptoms. A PCOS diet promotes a healthy relationship with food (rather than focusing on weight loss). This makes it much more suitable for previous “failed” dieters and those at risk of disordered eating.
The testimonies from my free 30-Day PCOS Diet Challenge show the superiority of this dietary approach.

For more information on how to lose weight with PCOS, see this article. Or if you’re trying to get pregnant, then here’s what you should read next.
Summary
A low-carb PCOS diet offers all the benefits of a keto diet but without the downsides.
The Bottom Line
The ketogenic diet may offer some short-term benefits for women with PCOS. This is especially the case for overweight women concerned about type 2 diabetes. But while this intervention may be helpful, a PCOS-focused diet can get even better results.
A PCOS diet is more sustainable and less risky, making it better suited as a long-term lifestyle intervention. Start your journey to better health and fertility by signing up for my free 30-Day PCOS Diet Challenge. If you aren’t ready to commit to 30 days try this free 3-Day Meal Plan instead.
Author
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.
Co-Authors

This blog post has been critically reviewed to ensure accurate interpretation and presentation of the scientific literature by Dr. Jessica A McCoy, Ph.D. Dr McCoy has a master’s degree in cellular and molecular biology, and a doctorate in reproductive biology and environmental health. She currently serves as a University professor at the College of Charleston, South Carolina.

This blog post has also been medically reviewed and approved by Dr. Sarah Lee, M.D. Dr. Lee is a board-certified Physician practicing with Intermountain Healthcare in Utah. She obtained a Bachelor of Science in Biology from the University of Texas at Austin before earning her Doctor of Medicine from UT Health San Antonio.
References
1Barrea, L., et al., Source and amount of carbohydrate in the diet and inflammation in women with polycystic ovary syndrome. Nutr Res Rev, 2018. 31(2): p. 291-301.
2Legro, R.S., et al., Prevalence and predictors of risk for type 2 diabetes mellitus and impaired glucose tolerance in polycystic ovary syndrome: a prospective, controlled study in 254 affected women. J Clin Endocrinol Metab, 1999. 84(1): p. 165-9.
3DeUgarte, C.M., A.A. Bartolucci, and R. Azziz, Prevalence of insulin resistance in the polycystic ovary syndrome using the homeostasis model assessment. Fertil Steril, 2005. 83(5): p. 1454-60.
4Fica, S., et al., Insulin resistance and fertility in polycystic ovary syndrome. J Med Life, 2008. 1(4): p. 415-22.
5Greenwood, E.A., et al., Insulin resistance is associated with depression risk in polycystic ovary syndrome. Fertil Steril, 2018. 110(1): p. 27-34.
6Batch, J.T., et al., Advantages and Disadvantages of the Ketogenic Diet: A Review Article. Cureus, 2020. 12(8): p. e9639.
7Stocker, R.K., et al., [Ketogenic Diet and its Evidence-Based Therapeutic Implementation in Endocrine Diseases]. Praxis (Bern 1994), 2019. 108(8): p. 541-553.
8Mavropoulos, J.C., et al., The effects of a low-carbohydrate, ketogenic diet on the polycystic ovary syndrome: a pilot study. Nutr Metab (Lond), 2005. 2: p. 35.
9Paoli, A., et al., Effects of a ketogenic diet in overweight women with polycystic ovary syndrome. J Transl Med, 2020. 18(1): p. 104.
10Cincione, R.I., et al., Effects of Mixed of a Ketogenic Diet in Overweight and Obese Women with Polycystic Ovary Syndrome. Int J Environ Res Public Health, 2021. 18(23).
11Ludwig, D.S., The Ketogenic Diet: Evidence for Optimism but High-Quality Research Needed. J Nutr, 2020. 150(6): p. 1354-1359.
12Cardoso-Silva, D., et al., Intestinal Barrier Function in Gluten-Related Disorders. Nutrients, 2019. 11(10).
13Arslan, N., E. Kose, and O. Guzel, The Effect of Ketogenic Diet on Serum Selenium Levels in Patients with Intractable Epilepsy. Biol Trace Elem Res, 2017. 178(1): p. 1-6.
14Bergqvist, A.G., et al., Selenium deficiency associated with cardiomyopathy: a complication of the ketogenic diet. Epilepsia, 2003. 44(4): p. 618-20.
15Sonnenburg, E.D. and J.L. Sonnenburg, Starving our microbial self: the deleterious consequences of a diet deficient in microbiota-accessible carbohydrates. Cell Metab, 2014. 20(5): p. 779-786.
16Lee, I., et al., Increased risk of disordered eating in polycystic ovary syndrome. Fertil Steril, 2017. 107(3): p. 796-802.
17Paganini, C., et al., The Overlap Between Binge Eating Behaviors and Polycystic Ovarian Syndrome: An Etiological Integrative Model. Curr Pharm Des, 2018. 24(9): p. 999-1006.
18Mady, M.A., et al., The ketogenic diet: adolescents can do it, too. Epilepsia, 2003. 44(6): p. 847-51.
19Mathieson, R.A., et al., The effect of varying carbohydrate content of a very-low-caloric diet on resting metabolic rate and thyroid hormones. Metabolism, 1986. 35(5): p. 394-8.
20Garelli, S., et al., High prevalence of chronic thyroiditis in patients with polycystic ovary syndrome. European Journal of Obstetrics & Gynecology and Reproductive Biology, 2013. 169(2): p. 248-251.
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.
Co-Authors

This blog post has been critically reviewed to ensure accurate interpretation and presentation of the scientific literature by Dr. Jessica A McCoy, Ph.D. Dr McCoy has a master’s degree in cellular and molecular biology, and a doctorate in reproductive biology and environmental health. She currently serves as a University professor at the College of Charleston, South Carolina.

This blog post has also been medically reviewed and approved by Dr. Sarah Lee, M.D. Dr. Lee is a board-certified Physician practicing with Intermountain Healthcare in Utah. She obtained a Bachelor of Science in Biology from the University of Texas at Austin before earning her Doctor of Medicine from UT Health San Antonio.