The Mediterranean diet has a nice emphasis on whole foods and has proven health benefits. But it needs to be fine-tuned for PCOS. Women with PCOS need a lower-carb Mediterranean diet. They should also avoid gluten and dairy, and hold a wider definition of “healthy fats”.
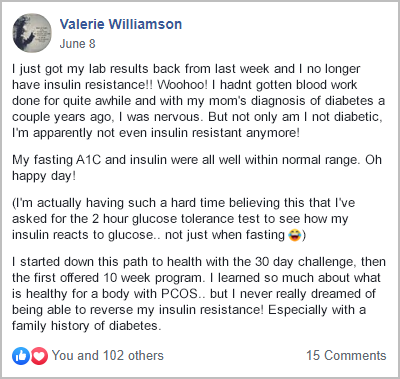
That’s what we do during my free 30-Day PCOS Diet Challenge. The results speak for themselves.

Here are the five pros and cons of the Mediterranean diet for PCOS.
Good Emphasis on Whole Foods
Proven Health Benefits
Too High in Carbs
Limited Definition of “Healthy Fat”
Includes Gluten and Dairy
1. Pro: Emphasis on Whole Foods
The best thing about the Mediterranean diet for PCOS is its emphasis on nutrient-dense whole foods. It’s old-fashioned eating created before the dawn of the processed food revolution. Most people would recognize the Mediterranean diet as a common-sense way to eat healthily.
The general guidelines are to:
- Have 5-10 servings per day of a wide variety of fruits and vegetables.
- Eat whole grains rather than refined grains as your main source of carbohydrates.
- Include beans, lentils, and chickpeas as these are high in protein, fiber, and micronutrients.
- Enjoy nuts and seeds in moderation.
- Use plenty of healthy fats from olive oil, avocados, and fatty fish.
- Eat fish and seafood at least twice a week.
- Limit red meat to less than once a week and choose lean cuts.
- Choose lean chicken and turkey meat.
- Eat cheese and low-fat yogurt in moderation.
- Use plenty of herbs and spices and limit salt.
2. Pro: Proven Health Benefits
The Mediterranean diet is one of the most well-studied diet patterns worldwide. This began in the 1950s when researchers noticed that people living in Greece and Italy had lower rates of heart disease and lived longer.
There’s strong evidence that the Mediterranean diet is good for cardiovascular health. It reduces risk factors such as obesity, hypertension, metabolic syndrome, and dyslipidemia [1, 2]. There’s also evidence that a Mediterranean diet is better for blood glucose control and lowers rates of type 2 diabetes.
These findings are particularly salient to people with PCOS. That’s because PCOS is a metabolic disease [3-5]. Studies show that the better people can follow a Mediterranean diet, the less severe their PCOS symptoms are [6].
3. Con: Too High in Carbs for PCOS
The Mediterranean diet is better for PCOS than the standard American diet. But that doesn’t mean it’s as good as it could be. One of the shortcomings is that it’s too high in carbs.
To be fair, the Mediterranean diet doesn’t have a prescribed macronutrient balance. But it’s typically around 45 – 55% carbs, 30-40% fat, and 15-20% protein. For PCOS women with insulin resistance, this is too many carbs to achieve optimal blood glucose levels. This limits your ability to manage PCOS symptoms by failing to address insulin resistance.
By modifying the macro balance of a Mediterranean diet, you can reverse insulin resistance. This makes a huge difference to your PCOS symptoms as well as your metabolic health. A recent study demonstrated this finding in overweight patients with PCOS. They found that a low-carb Mediterranean diet was better than a low-fat diet [7].
The importance of improving the macronutrient balance of your diet cannot be overstated. You can see the results of this intervention among participants from my free 30-Day PCOS Diet Challenge.
The best macros for PCOS are around 20% carbs, 60% fat, and 20% protein. In my carbs and PCOS article, I explain how best to achieve this balance.
4. Con: Limited on What Counts as a “Healthy Fat”
The Mediterranean diet promotes the consumption of certain high-fat foods. Nuts, seeds, olive oil, and fatty fish are encouraged. It’s fairly indisputable at this point that these are healthy foods.
But the Mediterranean diet is more cautious when it comes to meat. Chicken and eggs are meant to be eaten in moderation. You’re not supposed to eat red meat much at all. The general Mediterranean advice with meat is to always choose lean cuts.
This is a mistake for women with PCOS. For a start, eating fatty cuts of meat makes it much easier to achieve the best macros for PCOS. Changing macros improves insulin resistance more than a Mediterranean diet [8].
The health effects of whole food sources of animal fats have also been misrepresented by health authorities. For example, the weight of evidence now shows that saturated fat doesn’t increase heart disease risks [9]. Not all saturated fats are the same as some have positive health effects [10]. Experts argue that US government recommendations to limit saturated fats, ‘lacks scientific rigor’ [11].
From a practical perspective, you only need to look at the success of ketogenic diets in driving weight loss. I don’t support the use of a keto diet for PCOS. But it shows how dietary fat doesn’t make you fat.
There’s other compelling evidence supporting the health benefits of animal fat consumption:
- Fat consumption has a positive effect on satiety and appetite [12]. This can help with weight loss.
- CLA fats found in beef and lamb increase insulin sensitivity and reduce body fat [13-16].
- Red meat, especially from grass-fed animals, is a good source of omega-3 fatty acids. This can be particularly important for people that don’t eat enough oily fish [17].
The take-home here is that not all animal fats are unhealthy. If you can source high-quality, unprocessed meats, eating the fattiest cuts is likely to be good for your PCOS. That’s why I recommend meat in all my PCOS meal plans.
5. Con: It Includes Dairy and Gluten
The best PCOS diet excludes gluten and dairy. At least until you’ve completed an elimination diet like my free 30-Day PCOS Diet Challenge.
Inflammation is one of the underlying drivers of all PCOS symptoms [18-23]. More specially, inflammation caused by gut dysbiosis can account for all the characteristics of a PCOS diagnosis [24-26].
As explained in my article on gluten and PCOS, gluten-containing grains are a problem for many women with PCOS. Even if they’re not yet aware of it. Studies show that gluten can cause “leaky gut” in predisposed people [27]. It even negatively affects intestinal permeability in healthy people [28]. Gluten sensitivity is hard to diagnose. Yet, its predisposing factors are common within PCOS populations.
That’s why a gluten-elimination diet makes good sense before embracing some of the recommended grains in a Mediterranean diet.
A similar argument can be made for dairy. I explain this further in my article on PCOS and dairy.
The Bottom Line
The Mediterranean diet is a good place to start for the treatment of PCOS. But to get the best results, you need to make some PCOS-specific modifications. You want to include all the good parts of this diet, but avoid the bad.
Women with PCOS should eat fewer carbs than what’s “normal” for a Mediterranean diet. The reduction in carbs should be offset by increases in healthy fats. This includes fatty cuts of red meat, especially if they’re sourced from grass-fed animals.
Before embracing gluten and dairy, it’s best to investigate how these ingredients affect your gut health. Follow a gluten-free, dairy-free PCOS-friendly diet for a month or two first.
For help getting started, join my free 30-Day PCOS Diet Challenge.
For examples of a PCOS Mediterranean diet, download this free 3-Day Meal Plan. It includes recipes and a shopping list.
Author
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.
References
1Guasch-Ferré, M. and W.C. Willett, The Mediterranean diet and health: a comprehensive overview. J Intern Med, 2021. 290(3): p. 549-566.
2Papadaki, A., E. Nolen-Doerr, and C.S. Mantzoros, The Effect of the Mediterranean Diet on Metabolic Health: A Systematic Review and Meta-Analysis of Controlled Trials in Adults. Nutrients, 2020. 12(11).
3Escobar-Morreale, H.F., Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nat Rev Endocrinol, 2018. 14(5): p. 270-284.
4Sangaraju, S.L., et al., Cardio-Metabolic Disease and Polycystic Ovarian Syndrome (PCOS): A Narrative Review. Cureus, 2022. 14(5): p. e25076.
5Wang, J., et al., Hyperandrogenemia and insulin resistance: The chief culprit of polycystic ovary syndrome. Life Sciences, 2019. 236.
6Barrea, L., et al., Adherence to the Mediterranean Diet, Dietary Patterns and Body Composition in Women with Polycystic Ovary Syndrome (PCOS). Nutrients, 2019. 11(10).
7Mei, S., et al., Mediterranean Diet Combined With a Low-Carbohydrate Dietary Pattern in the Treatment of Overweight Polycystic Ovary Syndrome Patients. Front Nutr, 2022. 9: p. 876620.
8Tettamanzi, F., et al., A High Protein Diet Is More Effective in Improving Insulin Resistance and Glycemic Variability Compared to a Mediterranean Diet-A Cross-Over Controlled Inpatient Dietary Study. Nutrients, 2021. 13(12).
9Hamley, S., The effect of replacing saturated fat with mostly n-6 polyunsaturated fat on coronary heart disease: a meta-analysis of randomised controlled trials. Nutr J, 2017. 16(1): p. 30.
10Forouhi, N.G., et al., Differences in the prospective association between individual plasma phospholipid saturated fatty acids and incident type 2 diabetes: the EPIC-InterAct case-cohort study. Lancet Diabetes Endocrinol, 2014. 2(10): p. 810-8.
11Astrup, A., et al., Dietary Saturated Fats and Health: Are the U.S. Guidelines Evidence-Based? Nutrients, 2021. 13(10).
12Samra, R.A., Frontiers in Neuroscience Fats and Satiety, in Fat Detection: Taste, Texture, and Post Ingestive Effects, J.P. Montmayeur and J. le Coutre, Editors. 2010, CRC Press/Taylor & Francis Copyright © 2010, Taylor & Francis Group, LLC.: Boca Raton (FL).
13Ryder, J.W., et al., Isomer-specific antidiabetic properties of conjugated linoleic acid. Improved glucose tolerance, skeletal muscle insulin action, and UCP-2 gene expression. Diabetes, 2001. 50(5): p. 1149-57.
14Castro-Webb, N., E.A. Ruiz-Narváez, and H. Campos, Cross-sectional study of conjugated linoleic acid in adipose tissue and risk of diabetes. Am J Clin Nutr, 2012. 96(1): p. 175-81.
15Blankson, H., et al., Conjugated linoleic acid reduces body fat mass in overweight and obese humans. J Nutr, 2000. 130(12): p. 2943-8.
16Kennedy, A., et al., Antiobesity mechanisms of action of conjugated linoleic acid. J Nutr Biochem, 2010. 21(3): p. 171-9.
17Davis, H., et al., Nutritional Benefits from Fatty Acids in Organic and Grass-Fed Beef. Foods, 2022. 11(5).
18Aboeldalyl, S., et al., The Role of Chronic Inflammation in Polycystic Ovarian Syndrome-A Systematic Review and Meta-Analysis. Int J Mol Sci, 2021. 22(5).
19Dimitriadis, G.K., I. Kyrou, and H.S. Randeva, Polycystic Ovary Syndrome as a Proinflammatory State: The Role of Adipokines. Curr Pharm Des, 2016. 22(36): p. 5535-5546.
20Escobar-Morreale, H.F., M. Luque-Ramírez, and F. González, Circulating inflammatory markers in polycystic ovary syndrome: a systematic review and metaanalysis. Fertil Steril, 2011. 95(3): p. 1048-58.e1-2.
21González, F., Inflammation in Polycystic Ovary Syndrome: underpinning of insulin resistance and ovarian dysfunction. Steroids, 2012. 77(4): p. 300-5.
22Popovic, M., G. Sartorius, and M. Christ-Crain, Chronic low-grade inflammation in polycystic ovary syndrome: is there a (patho)-physiological role for interleukin-1? Seminars in Immunopathology, 2019. 41(4): p. 447-459.
23Rudnicka, E., et al., Chronic Low Grade Inflammation in Pathogenesis of PCOS. Int J Mol Sci, 2021. 22(7).
24Tremellen, K. and K. Pearce, Dysbiosis of Gut Microbiota (DOGMA)–a novel theory for the development of Polycystic Ovarian Syndrome. Med Hypotheses, 2012. 79(1): p. 104-12.
25He, F.F. and Y.M. Li, Role of gut microbiota in the development of insulin resistance and the mechanism underlying polycystic ovary syndrome: a review. J Ovarian Res, 2020. 13(1): p. 73.
26Li, G., et al., Alterations of Gut Microbiome and Fecal Fatty Acids in Patients With Polycystic Ovary Syndrome in Central China. Front Microbiol, 2022. 13: p. 911992.
27Caio, G., et al., Effect of Gluten-Free Diet on Gut Microbiota Composition in Patients with Celiac Disease and Non-Celiac Gluten/Wheat Sensitivity. Nutrients, 2020. 12(6).
28Hollon, J., et al., Effect of gliadin on permeability of intestinal biopsy explants from celiac disease patients and patients with non-celiac gluten sensitivity. Nutrients, 2015. 7(3): p. 1565-76.
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.