Key Takeaways
Metformin is one of the most commonly prescribed treatments for PCOS. But it shouldn’t be. In this article, I describe the failures and shortcomings of metformin for PCOS. I also describe better alternatives. Chief among them are dietary interventions.
This is an evidence-driven perspective. But you can see how the consequences play out among women that take part in my free 30-Day PCOS Diet Challenge.
1. It’s Not Recommended for Polycystic Ovarian Syndrome
Experts recommend against the use of metformin for PCOS without diabetes. Even if you have glucose intolerance and are prediabetic. It’s only supposed to be for patients with type 2 diabetes.
In 2003, Dr. Robert Barbieri authored a guide on the use of metformin therapy to treat PCOS [1]. Many prescribing physicians may still rely on this guidance.
But, by 2018, Barberi and his colleagues had changed their recommendations. Based on more recent data, they no longer recommend the use of metformin as a first-line therapy for, “any indication” [2].
You can refer your doctor to their review of the literature here.
2. It’s Only a Band-Aid for Polycystic Ovary Syndrome
Metformin is a band-aid solution for preventing diabetes. The same is true in the treatment of PCOS. It only lowers your insulin levels as long as you’re taking it daily.
In 2002, the Diabetes Prevention Program Research Group quantified these benefits. They found that over 3 years, metformin reduced the incidence of newly developed diabetes cases by 31% [3]. But in a follow-up study, the majority of the benefit didn’t persist when the treatment was stopped [4]. This means that unless you make other changes, you’ll need to take metformin for life.
The same researchers compared metformin to a diet and lifestyle intervention. Their “lifestyle group” enrolled in a 24-week program focusing on diet and exercise. This group reduced their risk of type 2 diabetes by 58% [3]. This was significantly better than the 31% achieved by the metformin group. After 15 years, the lifestyle program still proved to be better than metformin at preventing diabetes [5]. For women in this study, the lifestyle program was also better at reducing microvascular complications.
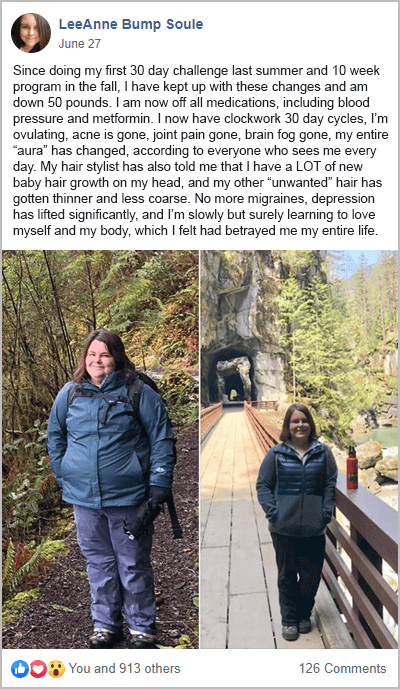
This supports what I see within my PCOS support group. Many women that take part in my free 30-Day PCOS Diet Challenge take metformin. For those that can adapt to a PCOS diet, their insulin sensitivity improves dramatically. Over time, many of these women get key biomarkers back within normal ranges and stop taking this unnecessary drug.
3. It Doesn’t Help with Weight Loss
Many women are told that metformin helps with weight loss. That’s why “metformin PCOS weight loss” and “PCOS belly fat metformin” are such heavily searched terms on Google. A quick look at the scientific literature though shows that any weight loss benefits of metformin for PCOS are small at best.
Metformin can cause weight loss in non-diabetic people. In one study, people with severe insulin resistance lost more weight than insulin-sensitive people [6]. These benefits were independent of age, sex, and BMI. But the results are different for women with PCOS.
In a 2017 meta-analysis, Morely and colleagues reviewed 42 metformin studies in women with PCOS. They found that metformin had a slight improvement in the distribution of excess body fat. This led to a small improvement in waist to hip ratio. But there was no effect on body weight [7].
Meta-analyses like these are the most powerful assessments of scientific evidence. Smaller (and older) metformin weight loss PCOS studies have shown a slight benefit [8]. But the size of the effect was small. When considering the entire body of evidence, metformin is unlikely to help you lose weight.
The impact of dietary change overshadows any potential gains. This is because managing your diet is the best way to reverse insulin resistance. The right diet can also address chronic inflammation. This is another underlying mechanism driving PCOS weight gain. You can see this at play when PCOS women lose weight during my free 30-Day PCOS Diet Challenge. Many of their other symptoms go away too.
Learn more about how to lose weight with PCOS here.
4. It Doesn’t Help Much with Fertility
Metformin is often used for treating anovulatory infertility in women with PCOS. It’s really common and I include myself in this cohort.
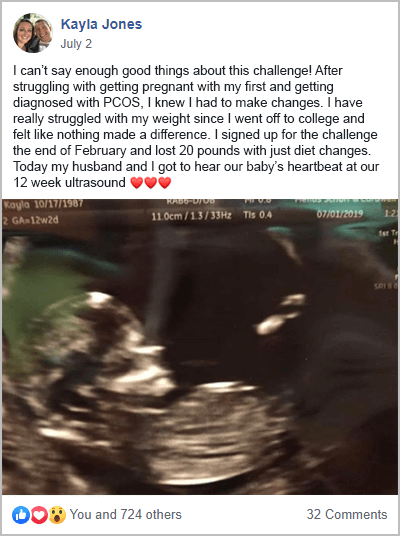
But the benefits of metformin for fertility are unclear. A 2019 review investigated the effectiveness of metformin for fertility treatment in women with PCOS. They found that for a live birth rate of 19% with no treatment, adding metformin could raise this rate by 0 to 18% [9]. This large range reflects the paucity of good data. It means that metformin therapy on it’s could have no benefit at all for fertility.
The potential benefits also seem to depend on your body weight. The quality of evidence is poor on this point too. But it appears that metformin is more likely to help non-obese PCOS women than those that are overweight [9].
The Endocrine Society Clinical Practice Guidelines state that “[metformin] has limited or no benefit in treating hirsutism, acne, or infertility [10].”
These statements would be more definitive if metformin improved PCOS infertility in a meaningful way. Given the alternatives, it’s likely that metformin will be seldom used for fertility treatment in the future.
The women from my PCOS community provide powerful testimony to the use of diet over metformin. Here are some examples from my free 30-Day PCOS Diet Challenge.
5. Metformin Depletes Nutrients
There’s a lot of evidence showing that metformin use is associated with decreased vitamin B12 status.
A study on older adults found that metformin use was the best predictor of vitamin B12 deficiency [11]. The larger the dose and the longer you use metformin, the lower your serum B12 levels are likely to be [12, 13]. This is because metformin impairs B12 absorption [14-18]. Given the importance of B12, this is bad news for women with PCOS. A sub-clinical deficiency can affect pregnancy outcomes, vascular, cognitive, bone, and eye health [19, 20].
Unfortunately, many women are not informed of this risk.
Metformin can also affect other vitamins and minerals. This includes vitamin B1, folic acid, vitamin D, and magnesium [21]. Nutrient supplements may be required especially if you’re trying to conceive.
Learn more about the importance of magnesium for PCOS here. This article on vitamin D for PCOS explains why this nutrient, in particular, should be at the top of the list for most people.
6. Side Effects Are Common
In one study, approximately 88% of people experienced metformin side effects [22]. The most common side effects include diarrhea, heartburn, nausea, abdominal pain, bloating, and retching [23].
When I polled my PCOS support Facebook group, 78% reported adverse effects. If you’re looking for metformin for PCOS reviews, here’s what some of the respondents said.
“I was violently sick and couldn’t eat, everyone thought I had morning sickness so I had to stop taking it”.
“It made me super sick and it was a terrible experience”.
“I was always sick to my stomach on it”.
“I had numerous side effects, tiredness, nauseous, headaches, pain in my abdomen.”
“the metformin I started taking for fertility made me bleed for over 20 days and I had to go to urgent care due to anemia.”
Metformin also has other less common side effects. Lactic acidosis is a rare but serious side effect [24]. There have been many case studies of metformin causing liver injury [25-27]. Studies on rats also suggest an increased risk of Alzheimer’s disease [28].
The take home here is that metformin may be a safer drug, but it’s not without its risks.
7. There Are Better Alternatives for Insulin Resistance
The effectiveness of alternatives to metformin for PCOS is one of the biggest reasons not to take this drug.
Inositol supplements show the most promise for PCOS. For example, inositol supplements are more effective than metformin at improving menstrual frequency [29].
A 2019 meta-analysis compared the insulin-sensitizing effects of myo-inositol and metformin. Again, myo-inositol was found to be as good as metformin. Myo-inositol also performed as well as metformin when it came to improving testosterone levels, body mass index, and more [30].
One argument in favor of metformin use is for reducing the risk of ovarian hyperstimulation syndrome during IVF [31]. But inositol supplements also offer this protection [32, 33].
The natural herb, berberine, also shows great potential in patients with PCOS. Trials show that it can improve insulin resistance, blood lipids, and ovulation [34-37]. Meta-analysis suggests that berberine is as effective as metformin for improving insulin sensitivity [38].
Like inositol supplements, berberine is generally well-tolerated. This means fewer side effects and less disruption to your everyday life. It’s important to keep in mind though, that berberine is not safe during pregnancy.
Metformin was first approved for us in 1994. This was back when PCOS was known as polycystic ovarian disease. Since then, many other insulin-sensitizing drugs have come to market. New treatments like Ozempic, Wegovy, and Mounjaro may be suitable alternatives. Especially for patients that can’t tolerate the side effects of metformin.
Of course, the best alternative to metformin for PCOS is changing how you eat. Metformin’s health benefits come from its anti-inflammatory and antioxidant properties [39]. Its alteration of the gut microbiome is also key to its effectiveness [40-42]. Both of these mechanisms depend on your diet.
A PCOS diet reduces inflammation and improves gut health. It can also reverse insulin resistance. By addressing the underlying causes of PCOS, the right diet can displace the need for metformin. It also improves other PCOS symptoms at the same time.
The Bottom Line
It’s hard to justify metformin treatment for PCOS. Experts in the field no longer recommend its use as a first-line therapy for PCOS patients. Even for PCOS women with diabetes, metformin is a band-aid solution with better alternatives.
Metformin doesn’t provide meaningful weight loss results. Its cost/benefit as a fertility treatment is also tenuous given the alternatives. Metformin depletes important nutrients and has significant side effects. Ovasitol and berberine perform just as well but are much better tolerated.
A PCOS diet is the most important step for improving insulin regulation and fertility. A PCOS diet can displace the need for metformin and can further improve other PCOS symptoms.
Start your journey to better health and fertility by signing up for my free 30-Day PCOS Diet Challenge. If you aren’t ready to commit to 30 days try this free 3-Day Meal Plan instead.
FAQ
Are there any foods to avoid when taking metformin for PCOS? Anyone with PCOS should reduce or avoid refined carbohydrates, sugar, and processed foods. But there’s no specific dietary change needed to take metformin. Learn more about the foods to avoid with PCOS here.
What does metformin do for PCOS? Insulin resistance causes or exacerbates symptoms in the majority of PCOS patients. Metformin is an insulin-sensitizing drug that works to reverse insulin resistance. But metformin has shown limited benefits in numerous studies of PCOS women. There are now many good alternatives to metformin for PCOS.
What about metformin for PCOS acne? Metformin is an effective treatment for PCOS acne [43]. But given the side effects, many people will prefer alternatives. Learn more about treating PCOS acne here.
Metformin vs birth control for PCOS. Metformin may be a suitable alternative to oral contraceptives for lowering androgen levels in PCOS patients [44]. This can help with hirsutism and acne. The relative risk differences regarding diabetes, cardiovascular disease, or endometrial cancer remain unknown [45].
How long does it take for metformin to work for PCOS? Metformin takes 2-3 months to work, although some changes may happen sooner. Early signs metformin is working for PCOS include more energy and reduced sugar cravings. Improvements in menstruation and acne are often also observed.
How long to take metformin for PCOS? Metformin is often used as a long-term treatment. That could mean many decades for some people. The diabetes prevention program has followed patients for more than 15 years [5].
What is the typical metformin dosage for PCOS? As well as getting the dose right it’s important to understand how to take metformin for PCOS. The starting dose for metformin is typically 250 mg taken twice a day. This should be gradually increased every 2 weeks to reach the desired therapeutic dose. The target dose for effectiveness is between 1500 -2500 mg/day. There’s no specific metformin dosage for PCOS weight loss.
What is the lowest dose of metformin you can take for PCOS? 1500 mg per day is the most common metformin dosage for PCOS used in clinical trials. Doses of 1000 mg per day have been used in trials when taking metformin and clomid together [46].
What happens if you miss a dose of metformin for PCOS? Provided your blood sugar levels are being managed, missing one dose shouldn’t matter too much. If it’s been less than a few hours since you missed the dose, take the missed dose right away. Otherwise, skip the dose and continue on your regular schedule at the next dose. Don’t take a double dose.
What to expect when taking metformin for PCOS. It’s common to experience side effects when starting metformin. Nausea and gut discomfort are particularly common.
Author
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.
Co-Authors

This blog post has been critically reviewed to ensure accurate interpretation and presentation of the scientific literature by Dr. Jessica A McCoy, Ph.D. Dr McCoy has a master’s degree in cellular and molecular biology, and a doctorate in reproductive biology and environmental health. She currently serves as a University professor at the College of Charleston, South Carolina.

This blog post has also been medically reviewed and approved by Dr. Sarah Lee, M.D. Dr. Lee is a board-certified Physician practicing with Intermountain Healthcare in Utah. She obtained a Bachelor of Science in Biology from the University of Texas at Austin before earning her Doctor of Medicine from UT Health San Antonio.
References
1Barbieri, R.L., Metformin for the treatment of polycystic ovary syndrome. Obstet Gynecol, 2003. 101(4): p. 785-93.
2Barbieri, R.L.E., D.A., Metformin for treatment of the polycystic ovary syndrome. UpToDate, 2018.
3Knowler, W.C., et al., Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med, 2002. 346(6): p. 393-403.
4Effects of withdrawal from metformin on the development of diabetes in the diabetes prevention program. Diabetes Care, 2003. 26(4): p. 977-80.
5Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol, 2015. 3(11): p. 866-75.
6Seifarth, C., B. Schehler, and H.J. Schneider, Effectiveness of metformin on weight loss in non-diabetic individuals with obesity. Exp Clin Endocrinol Diabetes, 2013. 121(1): p. 27-31.
7Morley, L.C., et al., Insulin-sensitising drugs (metformin, rosiglitazone, pioglitazone, D-chiro-inositol) for women with polycystic ovary syndrome, oligo amenorrhoea and subfertility. Cochrane Database Syst Rev, 2017. 11(11): p. Cd003053.
8Nieuwenhuis-Ruifrok, A.E., et al., Insulin sensitizing drugs for weight loss in women of reproductive age who are overweight or obese: systematic review and meta-analysis. Hum Reprod Update, 2009. 15(1): p. 57-68.
9Sharpe, A., et al., Metformin for ovulation induction (excluding gonadotrophins) in women with polycystic ovary syndrome. Cochrane Database Syst Rev, 2019. 12(12): p. Cd013505.
10Legro, R.S., et al., Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab, 2013. 98(12): p. 4565-92.
11Laird, E.J., et al., Voluntary fortification is ineffective to maintain the vitamin B12 and folate status of older Irish adults: evidence from the Irish Longitudinal Study on Ageing (TILDA). Br J Nutr, 2018. 120(1): p. 111-120.
12Aroda, V.R., et al., Long-term Metformin Use and Vitamin B12 Deficiency in the Diabetes Prevention Program Outcomes Study. J Clin Endocrinol Metab, 2016. 101(4): p. 1754-61.
13Ting, R.Z., et al., Risk factors of vitamin B(12) deficiency in patients receiving metformin. Arch Intern Med, 2006. 166(18): p. 1975-9.
14Bauman, W.A., et al., Increased intake of calcium reverses vitamin B12 malabsorption induced by metformin. Diabetes Care, 2000. 23(9): p. 1227-31.
15Kozyraki, R. and O. Cases, Vitamin B12 absorption: mammalian physiology and acquired and inherited disorders. Biochimie, 2013. 95(5): p. 1002-7.
16Wulffelé, M.G., et al., Effects of short-term treatment with metformin on serum concentrations of homocysteine, folate and vitamin B12 in type 2 diabetes mellitus: a randomized, placebo-controlled trial. J Intern Med, 2003. 254(5): p. 455-63.
17Quadros, E.V., Advances in the understanding of cobalamin assimilation and metabolism. Br J Haematol, 2010. 148(2): p. 195-204.
18Reinstatler, L., et al., Association of biochemical B₁₂ deficiency with metformin therapy and vitamin B₁₂ supplements: the National Health and Nutrition Examination Survey, 1999-2006. Diabetes Care, 2012. 35(2): p. 327-33.
19O’Leary, F. and S. Samman, Vitamin B12 in health and disease. Nutrients, 2010. 2(3): p. 299-316.
20Rogne, T., et al., Associations of Maternal Vitamin B12 Concentration in Pregnancy With the Risks of Preterm Birth and Low Birth Weight: A Systematic Review and Meta-Analysis of Individual Participant Data. Am J Epidemiol, 2017. 185(3): p. 212-223.
21Wakeman, M. and D.T. Archer, Metformin and Micronutrient Status in Type 2 Diabetes: Does Polypharmacy Involving Acid-Suppressing Medications Affect Vitamin B12 Levels? Diabetes Metab Syndr Obes, 2020. 13: p. 2093-2108.
22Florez, H., et al., Impact of metformin-induced gastrointestinal symptoms on quality of life and adherence in patients with type 2 diabetes. Postgrad Med, 2010. 122(2): p. 112-20.
23Bouchoucha, M., B. Uzzan, and R. Cohen, Metformin and digestive disorders. Diabetes Metab, 2011. 37(2): p. 90-6.
24Salpeter, S.R., et al., Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database Syst Rev, 2010. 2010(4): p. Cd002967.
25Hashmi, T., Probable hepatotoxicity associated with the use of metformin in type 2 diabetes. BMJ Case Rep, 2011. 2011.
26Saadi, T., et al., Metformin-induced mixed hepatocellular and cholestatic hepatic injury: case report and literature review. Int J Gen Med, 2013. 6: p. 703-6.
27Zheng, L., Metformin as a Rare Cause of Drug-Induced Liver Injury, a Case Report and Literature Review. Am J Ther, 2016. 23(1): p. e315-7.
28Picone, P., et al., Biological and biophysics aspects of metformin-induced effects: cortex mitochondrial dysfunction and promotion of toxic amyloid pre-fibrillar aggregates. Aging (Albany NY), 2016. 8(8): p. 1718-34.
29Zhao, H., et al., Comparative efficacy of oral insulin sensitizers metformin, thiazolidinediones, inositol, and berberine in improving endocrine and metabolic profiles in women with PCOS: a network meta-analysis. Reprod Health, 2021. 18(1): p. 171.
30Facchinetti, F., et al., Short-term effects of metformin and myo-inositol in women with polycystic ovarian syndrome (PCOS): a meta-analysis of randomized clinical trials. Gynecol Endocrinol, 2019. 35(3): p. 198-206.
31Wu, Y., et al., Association of Metformin With Pregnancy Outcomes in Women With Polycystic Ovarian Syndrome Undergoing In Vitro Fertilization: A Systematic Review and Meta-analysis. JAMA Netw Open, 2020. 3(8): p. e2011995.
32Merviel, P., et al., Impact of myo-inositol treatment in women with polycystic ovary syndrome in assisted reproductive technologies. Reprod Health, 2021. 18(1): p. 13.
33Turan, G.A., et al., Myo-inositol is a promising treatment for the prevention of ovarian hyperstimulation syndrome (OHSS): an animal study. Arch Gynecol Obstet, 2015. 292(5): p. 1163-71.
34Ju, J., et al., Efficacy and safety of berberine for dyslipidaemias: A systematic review and meta-analysis of randomized clinical trials. Phytomedicine, 2018. 50: p. 25-34.
35Rondanelli, M., et al., Polycystic ovary syndrome management: a review of the possible amazing role of berberine. Arch Gynecol Obstet, 2020. 301(1): p. 53-60.
36Wei, W., et al., A clinical study on the short-term effect of berberine in comparison to metformin on the metabolic characteristics of women with polycystic ovary syndrome. Eur J Endocrinol, 2012. 166(1): p. 99-105.
37Xie, L., et al., The Effect of Berberine on Reproduction and Metabolism in Women with Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis of Randomized Control Trials. Evid Based Complement Alternat Med, 2019. 2019: p. 7918631.
38Li, M.F., X.M. Zhou, and X.L. Li, The Effect of Berberine on Polycystic Ovary Syndrome Patients with Insulin Resistance (PCOS-IR): A Meta-Analysis and Systematic Review. Evid Based Complement Alternat Med, 2018. 2018: p. 2532935.
39Dehkordi, A.H., et al., Metformin and its anti-inflammatory and anti-oxidative effects; new concepts. Journal of Renal Injury Prevention, 2018.
40Wu, H., et al., Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug. Nat Med, 2017. 23(7): p. 850-858.
41Weersma, R.K., A. Zhernakova, and J. Fu, Interaction between drugs and the gut microbiome. Gut, 2020. 69(8): p. 1510-1519.
42Lee, C.B., et al., The Relationship between the Gut Microbiome and Metformin as a Key for Treating Type 2 Diabetes Mellitus. Int J Mol Sci, 2021. 22(7).
43Yen, H., et al., Metformin Therapy for Acne in Patients with Polycystic Ovary Syndrome: A Systematic Review and Meta-analysis. Am J Clin Dermatol, 2021. 22(1): p. 11-23.
44Johnson, N.P., Metformin use in women with polycystic ovary syndrome. Ann Transl Med, 2014. 2(6): p. 56.
45Costello, M., et al., Insulin-sensitising drugs versus the combined oral contraceptive pill for hirsutism, acne and risk of diabetes, cardiovascular disease, and endometrial cancer in polycystic ovary syndrome. Cochrane Database Syst Rev, 2007(1): p. Cd005552.
46Singh, I., et al., Increased pregnancy rates with metformin and clomiphene citrate in non-obese patients with polycystic ovary syndrome: prospective randomized study. Fertility and Sterility, 2001. 76(3, Supplement 1): p. S94.
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.
Co-Authors

This blog post has been critically reviewed to ensure accurate interpretation and presentation of the scientific literature by Dr. Jessica A McCoy, Ph.D. Dr McCoy has a master’s degree in cellular and molecular biology, and a doctorate in reproductive biology and environmental health. She currently serves as a University professor at the College of Charleston, South Carolina.

This blog post has also been medically reviewed and approved by Dr. Sarah Lee, M.D. Dr. Lee is a board-certified Physician practicing with Intermountain Healthcare in Utah. She obtained a Bachelor of Science in Biology from the University of Texas at Austin before earning her Doctor of Medicine from UT Health San Antonio.