Key Takeaways
Bloating and excess belly fat are the most common PCOS symptoms. Even lean women with PCOS often struggle with this symptom.
This article explains what a PCOS belly looks like. You’ll also learn how to get rid of PCOS belly using evidence-based lifestyle interventions.
As a companion to this article, I’ve created a free 3-Day Meal Plan that includes recipes and shopping list.
You can also sign-up for my free 30-Day PCOS Diet Challenge. This program includes meal plans, shopping lists, video lessons, and more. It’s now helped hundreds of thousands of women beat PCOS.
What Does a PCOS Belly Look Like?
Everyone wants to know what does a PCOS belly look like. In normal-weight women, having excess fat only on your tummy is a textbook sign of PCOS. But the reality is that there’s no stereotypical PCOS belly “look”. A PCOS belly shape can fit any of the examples shown in Figure 2.
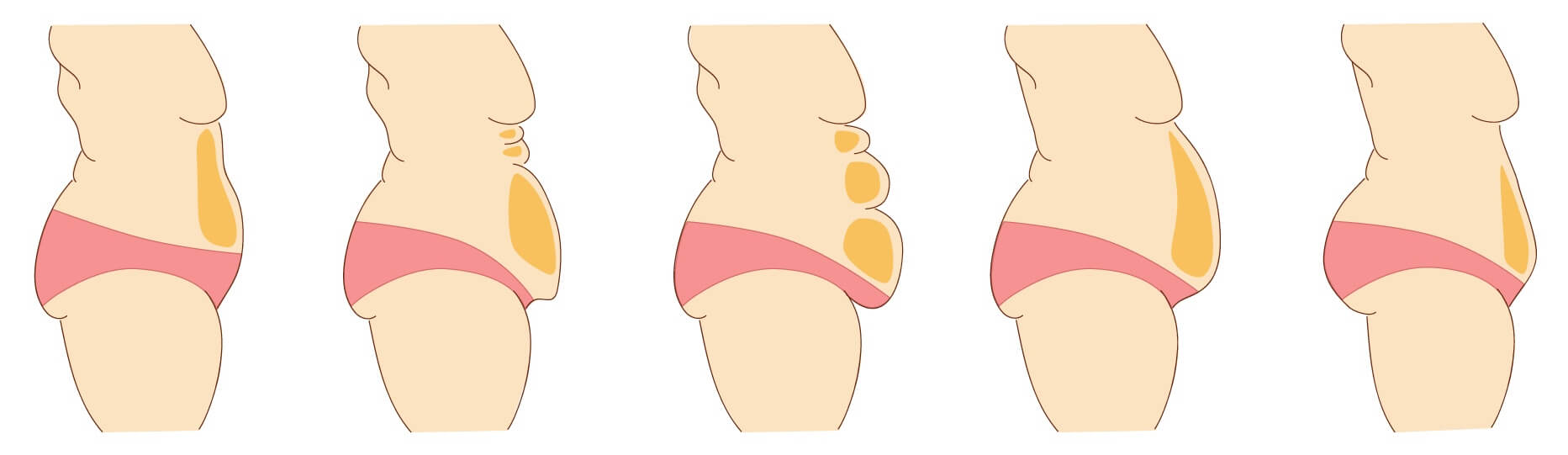
Figure 2. What’s your PCOS belly shape? All are possible as a result of this syndrome.
Because PCOS belly shape varies widely, this can create confusion. But the variability in PCOS belly shape is a consequence of the many different factors at play. Everything makes more sense when you understand the causes of PCOS belly.
Summary
There’s no one way for a PCOS belly to look. It depends on your unique diagnosis. Oftentimes, there’s a combination of factors that need to be parsed.
What is PCOS Belly?
PCOS belly is caused by three things. Bloating, subcutaneous fat, and visceral fat.
Bloating occurs when you have excess gas within your GI tract. This can be caused by irritable bowel syndrome or food sensitivities. Constipation or microbial overgrowths also cause bloating.
Subcutaneous fat is the fat you can see under your skin. It’s the soft stuff that you can pinch (or grab). Visceral fat, by contrast, is fat that sits around your organs.
Both subcutaneous and visceral fat are responsible for abdominal weight gain. But visceral fat is the more dangerous of the two. You can’t see visceral fat but it pushes your abdominal wall outwards. This creates the classic beer-belly look. The abdominal wall is made of muscle and tough fibrous tissue which is why visceral fat makes your abdomen hard.
Having a waist-to-hip ratio that’s more than 0.85 can be a useful diagnostic measure of polycystic ovary syndrome [48]. This is particularly useful for lean and normal-weight women.
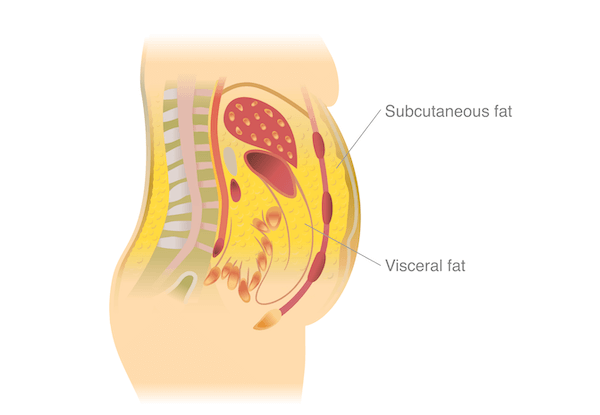
Figure 1. The different locations of subcutaneous and visceral fat.
For women with PCOS, bloating, subcutaneous fat, and visceral fat can all be an issue.
This creates confusion. But it’s also an opportunity for an easy win.
A lot of women join my free 30-Day PCOS Diet Challenge because they want to lose belly fat. Doing so in a healthy way is a slow and steady process. But bloating can often be addressed quickly. If you’re dealing with bacterial or fungal overgrowth things can take longer. But in most cases, dietary change can ease bloating within weeks, if not, days.
Relieving bloating reduces your waist circumference. Racking up some easy wins like this makes it easier to stick with the dietary changes that help with belly fat over the longer term.
Summary
PCOS belly can be caused by bloating, as well as excess abdominal weight gain. Bloating can often be addressed easily. Body composition is best improved over the long term.
Root Causes of PCOS Belly Fat
Women with PCOS have higher central abdominal fat deposits independent of body mass index [1].
This is why normal-weight women get a PCOS tummy too [2-4]. It’s also why the same PCOS diet works for all the different types of PCOS. Lean women tend to have a milder form of PCOS, but all PCOS phenotypes exist on the same spectrum. This means that the solution is the same too.
The root causes of PCOS are well understood. PCOS is driven by poor insulin regulation, elevated androgens, and chronic inflammation [5-10]. Diet is also a key factor in PCOS pathology [11].
Other factors contribute to PCOS belly fat too. Other hormonal imbalances relating to stress and cortisol responsiveness are strongly associated with abdominal obesity [12]. PCOS women may be particularly at risk here as studies show we have a “disturbed stress response” [13].
Thyroid dysfunction is another common underlying cause of PCOS belly fat. Autoimmune thyroiditis affects more than one in four women with PCOS [14, 15]. Many of these cases are undiagnosed.
Understanding these mechanisms points us toward the solutions to PCOS belly fat.
Summary
Poor insulin regulation, elevated androgens, and chronic inflammation cause PCOS belly. Diet is the best way to address these issues.
1. Regulate Insulin with Diet
Insulin resistance and body fat are intricately linked [16, 17]. Focusing on lifestyle changes that improve insulin sensitivity can solve both of these issues.
Following a PCOS diet is key. PCOS women with insulin resistance experience elevated insulin levels after consuming carbohydrate-rich foods. This is because one of insulin’s many roles is to transport glucose sugar from the blood into the body’s tissue where it’s either used or stored.
Research has shown that a typical Western diet is not appropriate for women with PCOS [11]. Most people eat too much sugar and carbs. What women with PCOS need instead is to eat fewer carbs sourced from low-GI whole foods. This usually means cutting sugar intake too.
Fats and proteins have minimal impact on blood sugar levels. Consuming healthy fats and protein with carbs slows the rate at which blood sugar levels rise. Dietary fiber also has this effect.
This is why it’s recommended that women with PCOS eat a low-carb, high-fat, adequate protein diet. I explain this further in my article on the best macros for PCOS. If you want to lose PCOS belly fat, then getting your macros right is essential.
For examples of what a macro-balanced PCOS diet looks like, download this free 3-Day Meal Plan. Or sign-up for my next free 30-Day PCOS Diet Challenge.
Summary
Altering your diet to better manage your blood sugar levels is the best way to improve insulin regulation. This is key for driving weight loss from the stomach.
2. Regulate Insulin with Supplements
Metformin is the most widely used pharmaceutical for improving insulin regulation in women with PCOS. But experts now warn against its use for this purpose. As I explain in my article on Metformin for PCOS, this drug doesn’t help you lose weight either.
Fortunately, other natural medicines may be better.
Inositol is one of the best supplements for PCOS. This class of vitamin-like compounds has insulin-regulating effects. But like metformin, the impact on PCOS related weight loss is small.
Berberine and Vitamin D are possibly the best PCOS belly supplements. As explained more in my article on Berberine for PCOS, this natural herb doesn’t promote weight loss overall. But it’s effective at reducing visceral fat [18]. It also improves insulin regulation and is well-demonstrated as an effective treatment [19, 20].
As I explain in my article on Vitamin D for PCOS, women with PCOS need to ensure they have adequate levels of this essential nutrient. Given its health-wide impact, insufficient vitamin D is a significant barrier to PCOS weight loss. Supplementation is required for most women.
Magnesium also appears to be important. Studies show that having normal magnesium levels is essential for optimal insulin regulation [21]. A recent review of the literature supported the importance of this mineral for women with PCOS. Magnesium combined with vitamin E or zinc-calcium-vitamin D improves metabolic health [22]. Women with PCOS have increased risks for mineral deficiencies [23]. Given this hazard, nutrient supplementation can be another easy win in your battle with a PCOS belly.
Learn more about the best supplements for PCOS here.
Summary
Several dietary supplements can further enhance insulin regulation. Inositol, berberine, vitamin D, and magnesium are among the most important supplements to consider.
3. Regulate Insulin with Lifestyle
Other lifestyle changes also improve insulin sensitivity.
The best exercise for PCOS belly fat is the exercise you do. That’s because both strength training and aerobic activity improve insulin sensitivity in women with PCOS [24-26]. So, find what you enjoy, and make a habit out of it. There’s no need to focus on specific exercises for PCOS belly. Things like planks and crunches etc. These types of exercise will help your muscle tone and strength. But they don’t result in any localized fat loss.
Intermittent fasting has also been demonstrated in PCOS populations. Limiting eating to within eight hours each day can improve body composition and insulin resistance. Menstruation, chronic inflammation, and androgen regulation can also be improved by fasting [27]. Learn more about what the science says on intermittent fasting for PCOS here.
Insufficient sleep is another risk factor for insulin resistance [28-30]. Better rest at night has many other benefits that can help you reduce belly fat. Inadequate sleep makes you less active and impacts your eating habits [31, 32]. For example, getting more sleep reduces sugar cravings [33, 34].
Summary
Exercise, intermittent fasting, and better sleep all improve insulin regulation. This can help reduce PCOS belly fat.
4. Lower Androgen Levels
Elevated androgens like testosterone are one of the hallmarks of a PCOS diagnosis. Elevated androgen levels are closely associated with insulin resistance. Some researchers believe these two factors are the main causes of PCOS [5].
This means that anything that lowers androgens can help with losing belly fat with PCOS. This is often the argument used for PCOS teas or anti-androgenic herbs for PCOS. These may help on the margins, but the strength of the effects is usually small.
The best way to lower androgens is to improve insulin sensitivity (see above). Reducing inflammation is also very powerful.
Summary
Lowering androgen levels can help relieve PCOS symptoms (including PCOS tummy fat). Anti-androgenic compounds have a small effect. But it’s more important to improve insulin regulation with diet and lifestyle changes.
5. Reduce Inflammation
Chronic inflammation is one of the underlying mechanisms that cause PCOS [6-11]. That’s why reducing inflammation helps with PCOS belly on several fronts.
Inflammation occurs when the body’s immune system is triggered. There are many ways that our everyday environment creates an inflammatory burden. Endocrine disruptors found throughout the household can exacerbate pre-existing PCOS inflammation. Other factors like poor air and water quality, or chronic infections also drive an inflammatory response.
The biggest source of inflammation for women with PCOS though occurs through the gut.
Inflammation occurs whenever intestinal permeability is compromised [35]. There are several common causes of increased gut permeability:
- Imbalances in the gut microbiome [36]
- Sugary foods [37]
- “Vegetable oils” [38]
- Gluten-containing foods [39, 40]
- Dairy products (for people with dairy intolerances) [41]
- Other food allergies or intolerances
- Heavily processed foods
The impact of these foods to avoid with PCOS guides the creation of my PCOS recipes. The meal plans I provide during my free 30-Day PCOS Diet Challenge are all gluten and dairy-free. Same with those in my free 3-Day Meal Plan. I don’t use vegetable oils and sugar is kept as low as practical. A healthy gut microbiome is also promoted through the consumption of prebiotic vegetables. The results speak for themselves.
Summary
Lowering your inflammatory burden can help reduce you PCOS belly. Minimize environmental exposures and improve gut health by avoiding inflammatory foods.
6. Relieve Stress
Stress and obesity are trapped in a vicious cycle. Obesity causes stress and stress causes obesity [42].
Stress causes abdominal fat accumulation by increasing cortisol secretion [43, 44]. It also alters our behavior making weight gain easier and weight loss harder [45].
Researchers have tried to break this cycle with evidence-based interventions. For example, a mindfulness program for stress eating showed some promise. Improvements in mindfulness, stress, and cortisol were associated with reductions in abdominal fat [46].
But there are many other practical ways to help relieve stress. Slow down, cut yourself some slack, and connect with the people you love. Getting more sleep and making time for exercise can also help.
Many women want to know if coffee is bad for PCOS. Your sensitivity to stress plays a large role in answering this question. From what I’ve seen in the laboratory of real life, among other things, quitting caffeine helps get rid of PCOS stomach fat.
Summary
Stress and excess stomach fat are intricately linked. Any step that reduces psychological stress can help reduce PCOS stomach fat.
7. Get Your Thyroid Sorted
Thyroid dysfunction is a common comorbidity of PCOS [14]. It’s also closely associated with obesity [47].
Because PCOS and thyroid dysfunction share so many similarities, a PCOS diet also helps with an underactive thyroid. But sometimes diet alone isn’t enough.
Depending on your circumstances, you may need medical assistance. This can further enhance your efforts to get rid of excess PCOS lower belly fat. To understand your unique requirements, it’s important to get a full thyroid panel. You don’t want to rely on the standard tests for TSH and T4. These thyroid biomarkers can be normal in women with PCOS despite an underlying thyroid disorder. A proper diagnosis can only be made with a thyroid panel that includes TBG, T3, reverse T3, and thyroid antibodies (TPOAb and TGAb).
Speak with your doctor about getting these tests.
Summary
It’s common for thyroid dysfunction to go undiagnosed in PCOS patients. This can make it particularly difficult to get rid of excess stomach fat. Insist your physician orders a full thyroid panel.
The Bottom Line
Bloating and excess stomach fat are common issues within the PCOS community. Bloating can often be resolved quickly. But a slow and steady approach is best for losing belly fat with PCOS.
Many interventions target the underlying causes of PCOS belly. Dietary change is the most important place to start. For help putting a PCOS diet into practice, sign-up now for my free 30-Day PCOS Diet Challenge. Or begin today with this free 3-Day Meal Plan.
Other lifestyle factors also play a role in reducing excess PCOS stomach fat. These include fasting, exercise, sleep, and stress reduction. If you need more help than what you can achieve on your own, speak with your doctor about a full thyroid function test. Nutritional supplements that can improve insulin sensitivity are also worth considering.
Author
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.
References
1Huang, Z.H., et al., PCOS is associated with increased CD11c expression and crown-like structures in adipose tissue and increased central abdominal fat depots independent of obesity. J Clin Endocrinol Metab, 2013. 98(1): p. E17-24.
2Pasquali, R. and C. Oriolo, Obesity and Androgens in Women. Front Horm Res, 2019. 53: p. 120-134.
3Dumesic, D.A., et al., Hyperandrogenism Accompanies Increased Intra-Abdominal Fat Storage in Normal Weight Polycystic Ovary Syndrome Women. J Clin Endocrinol Metab, 2016. 101(11): p. 4178-4188.
4Dumesic, D.A., et al., Accelerated subcutaneous abdominal stem cell adipogenesis predicts insulin sensitivity in normal-weight women with polycystic ovary syndrome. Fertil Steril, 2021. 116(1): p. 232-242.
5Wang, J., et al., Hyperandrogenemia and insulin resistance: The chief culprit of polycystic ovary syndrome. Life Sciences, 2019. 236.
6González, F., Inflammation in Polycystic Ovary Syndrome: underpinning of insulin resistance and ovarian dysfunction. Steroids, 2012. 77(4): p. 300-5.
7González, F., et al., Hyperandrogenism sensitizes mononuclear cells to promote glucose-induced inflammation in lean reproductive-age women. Am J Physiol Endocrinol Metab, 2012. 302(3): p. E297-306.
8Popovic, M., G. Sartorius, and M. Christ-Crain, Chronic low-grade inflammation in polycystic ovary syndrome: is there a (patho)-physiological role for interleukin-1? Seminars in Immunopathology, 2019. 41(4): p. 447-459.
9Rostamtabar, M., et al., Pathophysiological roles of chronic low-grade inflammation mediators in polycystic ovary syndrome. J Cell Physiol, 2021. 236(2): p. 824-838.
10Rudnicka, E., et al., Chronic Low Grade Inflammation in Pathogenesis of PCOS. Int J Mol Sci, 2021. 22(7).
11Barrea, L., et al., Source and amount of carbohydrate in the diet and inflammation in women with polycystic ovary syndrome. Nutr Res Rev, 2018. 31(2): p. 291-301.
12van der Valk, E.S., M. Savas, and E.F.C. van Rossum, Stress and Obesity: Are There More Susceptible Individuals? Curr Obes Rep, 2018. 7(2): p. 193-203.
13Benson, S., et al., Disturbed stress responses in women with polycystic ovary syndrome. Psychoneuroendocrinology, 2009. 34(5): p. 727-35.
14Garelli, S., et al., High prevalence of chronic thyroiditis in patients with polycystic ovary syndrome. European Journal of Obstetrics & Gynecology and Reproductive Biology, 2013. 169(2): p. 248-251.
15Romitti, M., et al., Association between PCOS and autoimmune thyroid disease: a systematic review and meta-analysis. Endocrine Connections, 2018. 7(11): p. 1158-1167.
16Patel, P. and N. Abate, Body fat distribution and insulin resistance. Nutrients, 2013. 5(6): p. 2019-27.
17Patel, P. and N. Abate, Role of subcutaneous adipose tissue in the pathogenesis of insulin resistance. J Obes, 2013. 2013: p. 489187.
18Rondanelli, M., et al., Polycystic ovary syndrome management: a review of the possible amazing role of berberine. Arch Gynecol Obstet, 2020. 301(1): p. 53-60.
19Zhang, S.W., et al., Effect and mechanism of berberine against polycystic ovary syndrome. Biomed Pharmacother, 2021. 138: p. 111468.
20Li, M.F., X.M. Zhou, and X.L. Li, The Effect of Berberine on Polycystic Ovary Syndrome Patients with Insulin Resistance (PCOS-IR): A Meta-Analysis and Systematic Review. Evid Based Complement Alternat Med, 2018. 2018: p. 2532935.
21Hosseini Dastgerdi, A., M. Ghanbari Rad, and N. Soltani, The Therapeutic Effects of Magnesium in Insulin Secretion and Insulin Resistance. Adv Biomed Res, 2022. 11: p. 54.
22Li, R., et al., The effect of magnesium alone or its combination with other supplements on the markers of inflammation, OS and metabolism in women with polycystic ovarian syndrome (PCOS): A systematic review. Front Endocrinol (Lausanne), 2022. 13: p. 974042.
23Szczuko, M., et al., Quantitative assessment of nutrition in patients with polycystic ovary syndrome (PCOS). Rocz Panstw Zakl Hig, 2016. 67(4): p. 419-426.
24Cheema, B.S., L. Vizza, and S. Swaraj, Progressive resistance training in polycystic ovary syndrome: can pumping iron improve clinical outcomes? Sports Med, 2014. 44(9): p. 1197-207.
25Almenning, I., et al., Effects of High Intensity Interval Training and Strength Training on Metabolic, Cardiovascular and Hormonal Outcomes in Women with Polycystic Ovary Syndrome: A Pilot Study. PLoS One, 2015. 10(9): p. e0138793.
26Covington, J.D., et al., Higher circulating leukocytes in women with PCOS is reversed by aerobic exercise. Biochimie, 2016. 124: p. 27-33.
27Li, C., et al., Eight-hour time-restricted feeding improves endocrine and metabolic profiles in women with anovulatory polycystic ovary syndrome. J Transl Med, 2021. 19(1): p. 148.
28Van Cauter, E., Sleep disturbances and insulin resistance. Diabet Med, 2011. 28(12): p. 1455-62.
29Nedeltcheva, A.V., et al., Exposure to recurrent sleep restriction in the setting of high caloric intake and physical inactivity results in increased insulin resistance and reduced glucose tolerance. J Clin Endocrinol Metab, 2009. 94(9): p. 3242-50.
30Tasali, E., et al., Impact of obstructive sleep apnea on insulin resistance and glucose tolerance in women with polycystic ovary syndrome. J Clin Endocrinol Metab, 2008. 93(10): p. 3878-84.
31Schmid, S.M., et al., Short-term sleep loss decreases physical activity under free-living conditions but does not increase food intake under time-deprived laboratory conditions in healthy men. Am J Clin Nutr, 2009. 90(6): p. 1476-82.
32Blumfield, M.L., et al., Dietary disinhibition mediates the relationship between poor sleep quality and body weight. Appetite, 2018. 120: p. 602-608.
33Smith, S.L., M.J. Ludy, and R.M. Tucker, Changes in taste preference and steps taken after sleep curtailment. Physiol Behav, 2016. 163: p. 228-233.
34Al Khatib, H.K., et al., Sleep extension is a feasible lifestyle intervention in free-living adults who are habitually short sleepers: a potential strategy for decreasing intake of free sugars? A randomized controlled pilot study. Am J Clin Nutr, 2018. 107(1): p. 43-53.
35Fasano, A., Zonulin and its regulation of intestinal barrier function: the biological door to inflammation, autoimmunity, and cancer. Physiol Rev, 2011. 91(1): p. 151-75.
36Tilg, H., et al., The intestinal microbiota fuelling metabolic inflammation. Nat Rev Immunol, 2020. 20(1): p. 40-54.
37Zhang, D.M., R.Q. Jiao, and L.D. Kong, High Dietary Fructose: Direct or Indirect Dangerous Factors Disturbing Tissue and Organ Functions. Nutrients, 2017. 9(4).
38DiNicolantonio, J.J. and J. O’Keefe, The Importance of Maintaining a Low Omega-6/Omega-3 Ratio for Reducing the Risk of Autoimmune Diseases, Asthma, and Allergies. Mo Med, 2021. 118(5): p. 453-459.
39Hollon, J., et al., Effect of gliadin on permeability of intestinal biopsy explants from celiac disease patients and patients with non-celiac gluten sensitivity. Nutrients, 2015. 7(3): p. 1565-76.
40Caio, G., et al., Effect of Gluten-Free Diet on Gut Microbiota Composition in Patients with Celiac Disease and Non-Celiac Gluten/Wheat Sensitivity. Nutrients, 2020. 12(6).
41Bordoni, A., et al., Dairy products and inflammation: A review of the clinical evidence. Crit Rev Food Sci Nutr, 2017. 57(12): p. 2497-2525.
42Kumar, R., M.R. Rizvi, and S. Saraswat, Obesity and Stress: A Contingent Paralysis. Int J Prev Med, 2022. 13: p. 95.
43Donoho, C.J., et al., Stress and abdominal fat: preliminary evidence of moderation by the cortisol awakening response in Hispanic peripubertal girls. Obesity (Silver Spring), 2011. 19(5): p. 946-52.
44Epel, E.S., et al., Stress and body shape: stress-induced cortisol secretion is consistently greater among women with central fat. Psychosom Med, 2000. 62(5): p. 623-32.
45Tomiyama, A.J., Stress and Obesity. Annu Rev Psychol, 2019. 70: p. 703-718.
46Daubenmier, J., et al., Mindfulness Intervention for Stress Eating to Reduce Cortisol and Abdominal Fat among Overweight and Obese Women: An Exploratory Randomized Controlled Study. J Obes, 2011. 2011: p. 651936.
47Song, R.H., et al., The Impact of Obesity on Thyroid Autoimmunity and Dysfunction: A Systematic Review and Meta-Analysis. Front Immunol, 2019. 10: p. 2349.
48Majumdar, A. and T.A. Singh, Comparison of clinical features and health manifestations in lean vs. obese Indian women with polycystic ovarian syndrome. J Hum Reprod Sci, 2009. 2(1): p. 12-7.
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.