Many women with PCOS suffer from bloating for far longer than is necessary. I see this all the time during my free 30-Day PCOS Diet Challenge. Sometimes dietary change is all that’s needed to overcome this problem for good.
Diet is certainly important. But there are many other solutions to PCOS bloating as explained below.
Root Causes of PCOS Bloating
Bloating is caused by a build-up of gas in your gastrointestinal tract. This over-production of gas is a result of disturbances to your gut microbiome. If you’re experiencing bloating, then you need to figure out what’s causing this disturbance.
Diet and/or food intolerances are the most common cause of bloating among women with PCOS. But the hormonal imbalances of PCOS also play a role. It’s common for women with PCOS to have elevated estrogen levels. Estrogen causes water retention in your uterus giving you a bloated abdomen. But estrogen can also affect your intestinal motility causing gas to accumulate. Couple that with pelvic floor dysfunction following pregnancy and you’ve got a good recipe for bloating.
Many commonly prescribed medications for PCOS are also known to cause bloating. GI discomfort is the most reported side-effect of Metformin [1]. Hormonal birth control can also cause bloating.
Pathogenic microorganisms are one of the least well-understood causes of bloating. Both fungal and bacterial overgrowths in the small intestine can cause unexplained GI symptoms [2, 3]. Undiagnosed parasitic infections are also more common than people think. For example, infections of Blastocystis, Dientamoeba, and Giardia are often missed in patients with IBS [4, 5].
An understanding of these root causes of PCOS bloating provides a foundation for seeking the right treatment.
1. Cut Out Problem Foods
Dietary interventions are essential for anyone with PCOS regardless of their presenting symptoms. A PCOS diet helps with weight management and fertility. It can also reduce acne, hirsutism, and hair loss.
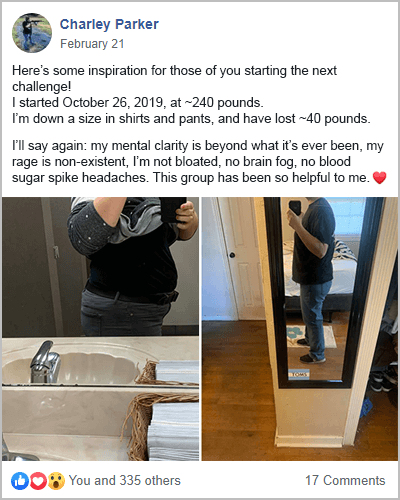
Many of the health benefits of a PCOS diet take months or even years to realize. But bloating is one symptom that can resolve quickly. Many participants in my free 30-Day PCOS Diet Challenge see reduced bloating as soon as they start following my meal plan.
Because a PCOS diet helps rebalance hormones, this can help with estrogen-dominance-related bloating. But the exclusion of problematic ingredients is likely what causes the quick results.
There are seven foods to avoid with PCOS. But gluten and dairy are the most obvious places to start for bloating. No matter the root cause of your bloating, it’ll be difficult to determine without cutting out gluten and dairy first.
This free 3-Day PCOS Meal Plan helps you conduct a simple elimination diet for bloating. It includes six popular gluten and dairy-free recipes from my free 30-Day Challenge.
2. Eat More Pre and Probiotic Foods
The health (or ill health) of the 38 trillion bugs [6] that inhabit your colon has a big impact on PCOS. Research shows that the underlying components of this syndrome may be caused by imbalances in the gut microbiome [7-9]. The gut microbiome is also the source of the intestinal gasses that cause bloating [10]. Under healthy conditions, the gasses produced by the microbiome don’t cause an issue. When bloating occurs, it means these bugs aren’t happy.
This is another reason why a PCOS diet should be the first-line intervention for bloating. Changing your diet rapidly and reproducibly changes your gut microbiome [11].
The best way to cultivate a healthy gut microbiome is by consuming more vegetables. Vegetables rich in prebiotics are especially good because these feed your good gut bacteria. Examples include asparagus, artichoke, beetroot, cabbage, garlic, and onions.
Probiotic foods can also be helpful. These provide live cultures of bacteria that can impact your gut microbiome. Examples of PCOS-friendly probiotic foods include coconut yogurt, tempeh, and miso. Unpasteurized pickled vegetables like sauerkraut and kimchi are also good probiotic foods.
Experimenting with increases in pre and probiotic foods can help diagnose the underlying cause of bloating. For example, if these foods make bloating worse, it may be because of a small intestine bacterial overgrowth.
3. Rule Out Medication Side Effects
When experiencing bloating it’s important to rule out your medications as the cause.
For example, there are many reasons to not take metformin for PCOS. GI discomfort is one of them. Estimates suggest around 25-30% of metformin patients experienced digestive side effects [12-14].
One of the biggest reasons people are reluctant to stop metformin is because they’re worried about blood sugar regulation. But as explained here, there are better solutions that can work just as well. The most evidence-based alternatives to metformin include inositol, berberine, and dietary changes.
Bloating may also be a reason to reconsider hormonal birth control. Many doctors will suggest switching medications. But given all the other reasons to avoid PCOS birth control, it may be worth stopping this treatment altogether. There are better ways to control PCOS symptoms and healthier ways to prevent pregnancy.
4. Make Lifestyle Changes
Poor diet and medications are the most likely contributors to PCOS bloating. But other simple lifestyle hacks can help ease this problem. These include:
- Squeezing half a lemon into a glass of water and drinking it first thing in the morning
- Avoiding carbonated drinks
- Increasing intake of potassium to reduce fluid retention
- Drinking herbal PCOS tea
Other core natural treatments for PCOS can also help with bloating. Improving sleep, exercise, and stress management habits is a good idea for anyone.
The only downside of these interventions is that the strength of the effect is likely to be small. If bloating persists, then professional help may be needed.
5. See The Right Kind of Doctor
Unfortunately, not all bloating is a simple fix. This is especially the case when the root cause of the bloating is microbial overgrowths, parasites, or IBS.
If tips 1-4 above don’t solve your problem, then it’s time to seek the help of a functional medicine or naturopathic doctor. These physicians can order diagnostic testing to determine the underlying cause of your GI problems. They can then provide guidance and treatment on how best to resolve this issue.
In the past, I suffered a range of GI-related disorders. Resolving these problems was the first step in my journey to beat PCOS. In my experience, functional medicine and naturopathic doctors have more to offer patients than gastroenterologists.
See the IFM Find a Practitioner tool for help finding a doctor near you.
The Bottom Line
Bloating is a common problem for women with PCOS that has many different causes. Figuring out what the underlying problem is, is key to finding the right treatment. Making dietary changes is the most obvious place to start because this can resolve the majority of cases. To get started on a PCOS diet today, download this free 3-Day PCOS Meal Plan. For a more immersive experience, you can also sign-up for my free 30-Day PCOS Diet Challenge.
If medication is the cause of your bloating, then it’s worth considering alternatives. Many simple lifestyle hacks can help ease bloating, but the strength of the effect is likely to be small. For persistent and severe bloating issues, the help of a functional medicine or naturopathic doctor may be required.
Author
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.
References
1Nabrdalik, K., et al., Gastrointestinal adverse events of metformin treatment in patients with type 2 diabetes mellitus: A systematic review, meta-analysis and meta-regression of randomized controlled trials. Front Endocrinol (Lausanne), 2022. 13: p. 975912.
2Rao, S.S.C. and J. Bhagatwala, Small Intestinal Bacterial Overgrowth: Clinical Features and Therapeutic Management. Clin Transl Gastroenterol, 2019. 10(10): p. e00078.
3Erdogan, A. and S.S. Rao, Small intestinal fungal overgrowth. Curr Gastroenterol Rep, 2015. 17(4): p. 16.
4Stark, D., et al., Irritable bowel syndrome: a review on the role of intestinal protozoa and the importance of their detection and diagnosis. Int J Parasitol, 2007. 37(1): p. 11-20.
5Yakoob, J., et al., Blastocystis hominis and Dientamoeba fragilis in patients fulfilling irritable bowel syndrome criteria. Parasitol Res, 2010. 107(3): p. 679-84.
6Sender, R., S. Fuchs, and R. Milo, Revised Estimates for the Number of Human and Bacteria Cells in the Body. PLoS Biol, 2016. 14(8): p. e1002533.
7Tremellen, K. and K. Pearce, Dysbiosis of Gut Microbiota (DOGMA)–a novel theory for the development of Polycystic Ovarian Syndrome. Med Hypotheses, 2012. 79(1): p. 104-12.
8He, F.F. and Y.M. Li, Role of gut microbiota in the development of insulin resistance and the mechanism underlying polycystic ovary syndrome: a review. J Ovarian Res, 2020. 13(1): p. 73.
9Li, G., et al., Alterations of Gut Microbiome and Fecal Fatty Acids in Patients With Polycystic Ovary Syndrome in Central China. Front Microbiol, 2022. 13: p. 911992.
10Scaldaferri, F., et al., Intestinal gas production and gastrointestinal symptoms: from pathogenesis to clinical implication. Eur Rev Med Pharmacol Sci, 2013. 17 Suppl 2: p. 2-10.
11David, L.A., et al., Diet rapidly and reproducibly alters the human gut microbiome. Nature, 2014. 505(7484): p. 559-63.
12Bouchoucha, M., B. Uzzan, and R. Cohen, Metformin and digestive disorders. Diabetes Metab, 2011. 37(2): p. 90-6.
13Long-term safety, tolerability, and weight loss associated with metformin in the Diabetes Prevention Program Outcomes Study. Diabetes Care, 2012. 35(4): p. 731-7.
14Dujic, T., et al., Association of Organic Cation Transporter 1 With Intolerance to Metformin in Type 2 Diabetes: A GoDARTS Study. Diabetes, 2015. 64(5): p. 1786-93.
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.



