Pain is an often-overlooked aspect of PCOS. Yet it has a big impact on quality of life.
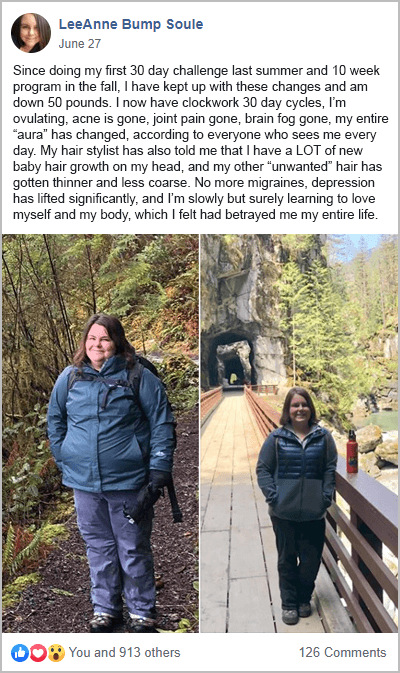
Systemic inflammation is the underlying driver of all types of PCOS pain. This is why a PCOS diet and lifestyle changes can reduce pain symptoms. Many women that take part in my free 30-Day PCOS Diet Challenge discover this for themselves.
Other innovative approaches can also help ease pain. These are discussed further below.
Does PCOS Cause Pain?
It’s been well documented that PCOS women experience more pain than is normal [1].
The exact types of pain aren’t well studied. But it’s well known that PCOS women suffer from cramping, painful periods, and heavy bleeding [2]. PCOS-related pain isn’t just limited to pelvic pain though. It can also be experienced in the neck, back, breasts, stomach, legs, and joints.
Part of this problem is pain caused by PCOS-related hormone imbalances. But PCOS women are also more prone to other pain-inducing problems. This includes:
- Endometriosis [3]
- Migraines [4]
- Fibromyalgia [5]
- Irritable Bowel Syndrome [6-8]
- Rheumatoid arthritis [9]
- Pain during sex [10]
Mental health issues can also exacerbate pain perception [11, 12].
Regardless of the type of pain, inflammation is at the heart of the problem. Inflammation is the immune system’s response to a perceived threat. It’s supposed to be a temporary state that promotes healing. In the case of PCOS though, low-grade inflammation persists over time [13-20]. Inflammation plays a key role in the development and maintenance of pain [21-23]. The more inflammation you experience, the more likely you are to experience pain.
Chronic inflammation has further problems in the context of PCOS. Inflammation exacerbates insulin resistance and drives up androgen levels. These three factors are the primary mechanisms behind all PCOS symptoms [17, 20, 24-26]. It’s also the downstream effects of these factors that cause PCOS pain.
For example, there is data to suggest that obesity, infertility, and hirsutism affect pain perception in PCOS women pain [1]. Inflammation, insulin resistance, and elevated androgens are also responsible for painful ovarian cysts.
Root-Cause Treatments for PCOS Pain
Addressing the underlying causes of PCOS is the best way to prevent and minimize PCOS-associated pain. There are many evidence-based ways to do this.
A PCOS diet is the most important place to start. It’s well known that dietary habits can promote inflammation and insulin resistance in PCOS [27-30]. This is the cause of all PCOS symptoms including irregular periods, weight gain, hirsutism, acne, and hair loss. As we see during my free 30-Day PCOS Diet Challenge, changing your diet can reverse these symptoms.
With knowledge of the foods to avoid with PCOS, systemic inflammation can be greatly reduced. Changing your food portions to achieve better macros for PCOS is also a powerful way to reverse insulin resistance.
Other systemic PCOS natural treatments include:
- Taking Ovasitol for PCOS
- Supplementing with vitamin D for PCOS
- Improving sleep quality
- Exercising
- Reducing stress
- Avoiding endocrine-disrupting chemicals
- Minimizing other environmental toxins (especially in drinking water)
Alternative PCOS Pain Relief
Most women will turn to over-the-counter pain relief when experiencing PCOS-related pain. For example, Advil (Nurofen) and Tylenol (Panadol) are often recommended. But some people have legitimate concerns regarding the safety of these medications [31, 32].
Several supplements may be as good for relieving pain but with fewer side effects. Curcumin, Fish Oil and pineapple-extracted Bromelain are the most well-studied. These supplements have outperformed non-steroid anti-inflammatory drugs, like Advil, in many trials [33-38].
Curcumin products containing the proprietary formulation, Meriva, offer a suitable alternative to Tylenol. In a comparison pain-relief trial, 2 grams of Meriva was comparable to two Tylenol Extra Strength tablets [39].
Innovative Pain Management Tools
Many novel pain management tools can help ease all types of PCOS pain.
The Wim Hoff Method, for example, shows a wide range of health benefits, including pain suppression. This approach is based on breathing exercises and cold therapy. Recent research shows that the Wim Hoff Method reduces inflammation [40, 41]. It’s also easy to learn within 2 hours of training.
Meditation is a component of the Wim Hoff Method. But meditation alone can also reduce pain. For example, an 8-week mindfulness-based stress reduction (MBSR) program has significant scientific credibility. MBSR can reduce inflammation in patients with lower back pain [42]. Meta-analysis shows that eight weeks of MBSR helps people with lower back pain for at least six months [43]. It’s been shown to help with irritable bowel syndrome and fibromyalgia [44]. MBSR has also proven effective in reducing pelvic pain in women [45].
For women with acute pain, there are many other innovative interventions worth exploring. These include:
The Bottom Line
PCOS pain is an ongoing problem that comes in many different forms. But it doesn’t need to be. Inflammation is the underlying mechanism behind all PCOS pain. This can be fixed with diet and lifestyle interventions.
Some plant-derived products can serve as an alternative to over-the-counter pain relief. There are many other ways to better manage pain. Some of the most innovative treatments include the Wim Hoff Method and other alternative therapies.
To start implementing a PCOS diet, join my free 30-Day PCOS Diet Challenge. Or try this free 3-Day meal plan first.
Author
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.
References
1Lu, K.T., et al., Evaluation of Bodily Pain Associated with Polycystic Ovary Syndrome: A Review of Health-Related Quality of Life and Potential Risk Factors. Biomedicines, 2022. 10(12).
2Martin, M.L., et al., Understanding polycystic ovary syndrome from the patient perspective: a concept elicitation patient interview study. Health Qual Life Outcomes, 2017. 15(1): p. 162.
3Hager, M., et al., The Prevalence of Incidental Endometriosis in Women Undergoing Laparoscopic Ovarian Drilling for Clomiphene-Resistant Polycystic Ovary Syndrome: A Retrospective Cohort Study and Meta-Analysis. J Clin Med, 2019. 8(8).
4Sarahian, N., et al., Is there any association between migraine headache and polycystic ovary syndrome (PCOS)? A review article. Mol Biol Rep, 2022. 49(1): p. 595-603.
5Pappolla, M.A., et al., Insulin Resistance is Associated with Central Pain in Patients with Fibromyalgia. Pain Physician, 2021. 24(2): p. 175-184.
6Bazarganipour, F., et al., The impact of irritable bowel syndrome on health-related quality of life in women with polycystic ovary syndrome. Health Qual Life Outcomes, 2020. 18(1): p. 226.
7Kałużna, M., et al., Are patients with polycystic ovary syndrome more prone to irritable bowel syndrome? Endocr Connect, 2022. 11(4).
8Tseng, P.H., et al., Obesity Exacerbates Irritable Bowel Syndrome-Related Sleep and Psychiatric Disorders in Women With Polycystic Ovary Syndrome. Front Endocrinol (Lausanne), 2021. 12: p. 779456.
9Sharmeen, S., et al., Polycystic ovary syndrome: epidemiologic assessment of prevalence of systemic rheumatic and autoimmune diseases. Clin Rheumatol, 2021. 40(12): p. 4837-4843.
10Loh, H.H., et al., Sexual dysfunction in polycystic ovary syndrome: a systematic review and meta-analysis. Hormones (Athens), 2020. 19(3): p. 413-423.
11Bair, M.J., et al., Depression and pain comorbidity: a literature review. Arch Intern Med, 2003. 163(20): p. 2433-45.
12Michaelides, A. and P. Zis, Depression, anxiety and acute pain: links and management challenges. Postgrad Med, 2019. 131(7): p. 438-444.
13Aboeldalyl, S., et al., The Role of Chronic Inflammation in Polycystic Ovarian Syndrome-A Systematic Review and Meta-Analysis. Int J Mol Sci, 2021. 22(5).
14Dimitriadis, G.K., I. Kyrou, and H.S. Randeva, Polycystic Ovary Syndrome as a Proinflammatory State: The Role of Adipokines. Curr Pharm Des, 2016. 22(36): p. 5535-5546.
15Escobar-Morreale, H.F., M. Luque-Ramírez, and F. González, Circulating inflammatory markers in polycystic ovary syndrome: a systematic review and metaanalysis. Fertil Steril, 2011. 95(3): p. 1048-58.e1-2.
16Carvalho, L.M.L., et al., Polycystic Ovary Syndrome as a systemic disease with multiple molecular pathways: a narrative review. Endocr Regul, 2018. 52(4): p. 208-221.
17González, F., Inflammation in Polycystic Ovary Syndrome: underpinning of insulin resistance and ovarian dysfunction. Steroids, 2012. 77(4): p. 300-5.
18Popovic, M., G. Sartorius, and M. Christ-Crain, Chronic low-grade inflammation in polycystic ovary syndrome: is there a (patho)-physiological role for interleukin-1? Seminars in Immunopathology, 2019. 41(4): p. 447-459.
19Rostamtabar, M., et al., Pathophysiological roles of chronic low-grade inflammation mediators in polycystic ovary syndrome. J Cell Physiol, 2021. 236(2): p. 824-838.
20Rudnicka, E., et al., Chronic Low Grade Inflammation in Pathogenesis of PCOS. Int J Mol Sci, 2021. 22(7).
21Voscopoulos, C. and M. Lema, When does acute pain become chronic? Br J Anaesth, 2010. 105 Suppl 1: p. i69-85.
22Baral, P., S. Udit, and I.M. Chiu, Pain and immunity: implications for host defence. Nat Rev Immunol, 2019. 19(7): p. 433-447.
23Watkins, L.R., E.D. Milligan, and S.F. Maier, Glial proinflammatory cytokines mediate exaggerated pain states: implications for clinical pain. Adv Exp Med Biol, 2003. 521: p. 1-21.
24Barrea, L., et al., Source and amount of carbohydrate in the diet and inflammation in women with polycystic ovary syndrome. Nutr Res Rev, 2018. 31(2): p. 291-301.
25Matulewicz, N. and M. Karczewska-Kupczewska, Insulin resistance and chronic inflammation. Postepy Hig Med Dosw (Online), 2016. 70(0): p. 1245-1258.
26Baillargeon, J.P. and A. Carpentier, Role of insulin in the hyperandrogenemia of lean women with polycystic ovary syndrome and normal insulin sensitivity. Fertil Steril, 2007. 88(4): p. 886-93.
27González, F., et al., Hyperglycemia alters tumor necrosis factor-alpha release from mononuclear cells in women with polycystic ovary syndrome. J Clin Endocrinol Metab, 2005. 90(9): p. 5336-42.
28González, F., et al., Reactive oxygen species-induced oxidative stress in the development of insulin resistance and hyperandrogenism in polycystic ovary syndrome. J Clin Endocrinol Metab, 2006. 91(1): p. 336-40.
29González, F., et al., Increased activation of nuclear factor kappaB triggers inflammation and insulin resistance in polycystic ovary syndrome. J Clin Endocrinol Metab, 2006. 91(4): p. 1508-12.
30González, F., et al., In vitro evidence that hyperglycemia stimulates tumor necrosis factor-alpha release in obese women with polycystic ovary syndrome. J Endocrinol, 2006. 188(3): p. 521-9.
31Minhas, D., A. Nidhaan, and M.E. Husni, Recommendations for the Use of Nonsteroidal Anti-inflammatory Drugs and Cardiovascular Disease Risk: Decades Later, Any New Lessons Learned? Rheum Dis Clin North Am, 2023. 49(1): p. 179-191.
32Ishitsuka, Y., Y. Kondo, and D. Kadowaki, Toxicological Property of Acetaminophen: The Dark Side of a Safe Antipyretic/Analgesic Drug? Biol Pharm Bull, 2020. 43(2): p. 195-206.
33Hsiao, A.F., et al., The efficacy of high- and low-dose curcumin in knee osteoarthritis: A systematic review and meta-analysis. Complement Ther Med, 2021. 63: p. 102775.
34Paultre, K., et al., Therapeutic effects of turmeric or curcumin extract on pain and function for individuals with knee osteoarthritis: a systematic review. BMJ Open Sport Exerc Med, 2021. 7(1): p. e000935.
35Maroon, J.C., J.W. Bost, and A. Maroon, Natural anti-inflammatory agents for pain relief. Surg Neurol Int, 2010. 1: p. 80.
36Muhammad, Z.A. and T. Ahmad, Therapeutic uses of pineapple-extracted bromelain in surgical care – A review. J Pak Med Assoc, 2017. 67(1): p. 121-125.
37Maroon, J.C. and J.W. Bost, Omega-3 fatty acids (fish oil) as an anti-inflammatory: an alternative to nonsteroidal anti-inflammatory drugs for discogenic pain. Surg Neurol, 2006. 65(4): p. 326-31.
38Zafari, M., F. Behmanesh, and A. Agha Mohammadi, Comparison of the effect of fish oil and ibuprofen on treatment of severe pain in primary dysmenorrhea. Caspian J Intern Med, 2011. 2(3): p. 279-82.
39Di Pierro, F., et al., Comparative evaluation of the pain-relieving properties of a lecithinized formulation of curcumin (Meriva(®)), nimesulide, and acetaminophen. J Pain Res, 2013. 6: p. 201-5.
40Kox, M., et al., Voluntary activation of the sympathetic nervous system and attenuation of the innate immune response in humans. Proc Natl Acad Sci U S A, 2014. 111(20): p. 7379-84.
41waag, J., et al., The Effects of Cold Exposure Training and a Breathing Exercise on the Inflammatory Response in Humans: A Pilot Study. Psychosom Med, 2022. 84(4): p. 457-467.
42Diez, G.G., et al., The effect of mindfulness on the inflammatory, psychological and biomechanical domains of adult patients with low back pain: A randomized controlled clinical trial. PLoS One, 2022. 17(11): p. e0276734.
43Soundararajan, K., V. Prem, and T.J. Kishen, The effectiveness of mindfulness-based stress reduction intervention on physical function in individuals with chronic low back pain: Systematic review and meta-analysis of randomized controlled trials. Complement Ther Clin Pract, 2022. 49: p. 101623.
44Islam, Z., et al., The role of mind body interventions in the treatment of irritable bowel syndrome and fibromyalgia. Front Psychiatry, 2022. 13: p. 1076763.
45Crisp, C.D., et al., Complementary Approaches for Military Women with Chronic Pelvic Pain: A Randomized Trial. J Integr Complement Med, 2023. 29(1): p. 22-30.
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.