This has to be one of the most important questions for women with PCOS.
The short answer is yes. PCOS is one of the most common causes of infertility, but it’s also easy to treat. The nuances of this answer though need a dive into the scientific literature.
Approximately 70-80% of women with PCOS experience infertility [1, 2]. But as you’ll see, this doesn’t need to be the case. After making the right diet and lifestyle changes, the chances of falling pregnant with PCOS can be better than average.
More often than not, changing how you eat is all that’s needed. This can be seen in the hundreds of success stories coming out of my free 30-Day PCOS Diet Challenge.
Get a taste of what a PCOS diet looks like by downloading this free 3-Day Meal Plan.
What Is PCOS?
The most important thing to know about PCOS is that inflammation and poor insulin regulation are the primary drivers of all symptoms [3-9]. Because of their effects on gut health, diet and lifestyle play an important role in PCOS pathology [10]. Dysbiosis of our gut microbiome can account for all three components of a PCOS diagnosis [11, 12]. These being irregular periods, elevated androgen levels, and polycystic ovaries.
Addressing gut health through diet and lifestyle can make the symptoms go away. And that’s crucial for getting pregnant with PCOS.
How PCOS Affects Fertility
Unmanaged PCOS has many negative effects on fertility.
PCOS impairs ovulation and reduces egg quality [13-16]. Being overweight makes this problem worse [15, 17, 18]. That’s why restoring a regular period is an essential milestone when treating PCOS with diet. For many women, losing weight is an important part of this process.
PCOS also makes the womb less receptive during implantation [12, 19]. This is another area where being overweight provides a further disadvantage [20]. Studies on weight-loss programs have shown how this can be repaired through diet [21].
Women with PCOS also experience higher rates of miscarriage. A recent meta-analysis on IVF patients suggests the risk of miscarriage is about 40-60% higher for PCOS women [22, 23]. This is a problem for lean women with PCOS too [24].
How Diet and Lifestyle Affect PCOS Infertility
Unmanaged PCOS is clearly a significant barrier to pregnancy. Approximately two-thirds of PCOS women don’t ovulate regularly [25]. Estimates suggest that 70-80% of women with PCOS will experience infertility [1, 2].
But your lifestyle choices can fix these problems. Poor PCOS statistics are only relevant to the general PCOS population. For the most part, these women are not implementing diet and lifestyle interventions.
PCOS affects fertility because of insulin resistance, inflammation, and elevated androgens. These factors are mediated by diet and gut health. This is why dietary change is the most important treatment for PCOS infertility. It’s also why exercise and stress management helps too.
The reality is that most of the dietary advice given to women with PCOS is not very good. Yet, despite these limitations, the impact of diet on PCOS infertility can still be seen in scientific studies.
A 2019 meta-analysis showed that lifestyle interventions improve androgen levels and body weight [26]. That’s good for PCOS fertility [27]. Another showed that diet improved reproductive outcomes in women with PCOS. Dietary change improves pregnancy rates and reduces miscarriage rates [28]. Further analysis showed that low-carbohydrate diets are the best for optimizing fertility. The longer the diet is maintained, the better the outcomes. Others have fine-tuned this advice by showing that increasing protein and switching to low-GI carbs is best for fertility [29].
These ideas are core aspects of my free 30-Day PCOS Diet Challenge. The results of these diet changes speak for themselves.
Chances of Getting Pregnant with PCOS Naturally
Non-PCOS population statistics can be used to understand your chances of getting pregnant with PCOS naturally. But only if you get your PCOS under control first. Boston University’s School of Public Health provides some of the best natural fertility data.
Figure 1 shows the pregnancy rates of 2962 couples that tried to conceive naturally between 2013 and 2017. These results show the percentage of women that fell pregnant after 6 and 12 months.
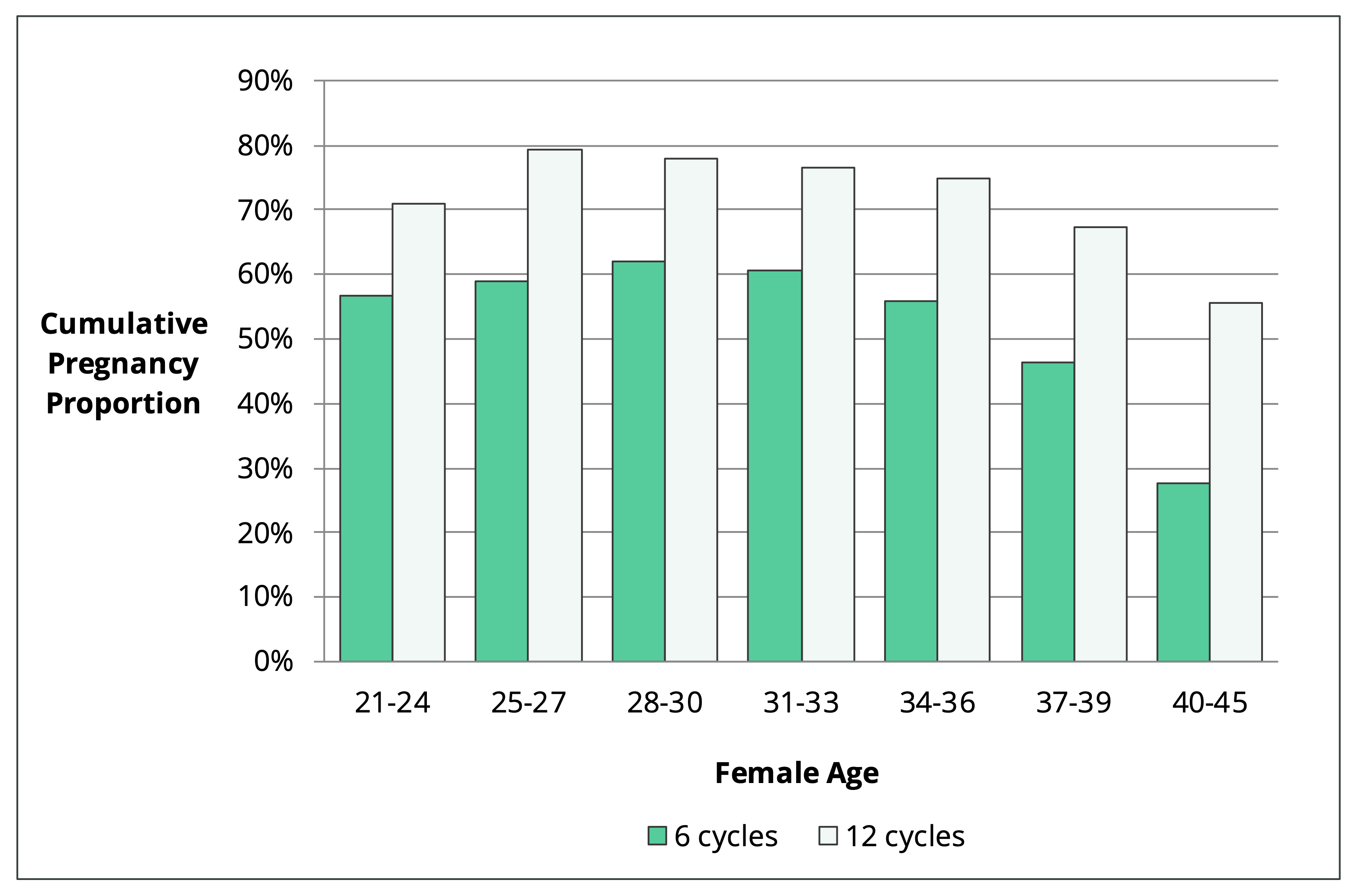
Figure 1. Cumulative pregnancy proportion within 6 and 12 cycles by female age [30].
There are a couple of key findings from this research. They showed that female fertility is stable until your mid-30s. They also showed that more than half of women in their early 40s will fall pregnant after 12 months of trying. This is approximately three-quarters the probability of women in their twenties.
During further analysis, these researchers showed that, based on age alone, women in their early 30’s had about 82% of the fertility of younger women. The reason that their pregnancy rates were higher though was because of all the other factors that enhance fertility. For example, female age was associated with:
- Previous pregnancy and childbirth.
- Improved regularity and length of cycle.
- Doing things that improve chances of conception. This included recording basal body temperature, monitoring cervical mucus, and using an ovulation predictor kit.
- Being a non-smoker and drinking less alcohol.
Another team of researchers considered natural fertility in terms of how long it takes to get pregnant. They analyzed the results from 1264 Japanese couples that were trying to have their first child. The outcomes for various age groups are shown in Figure 2.
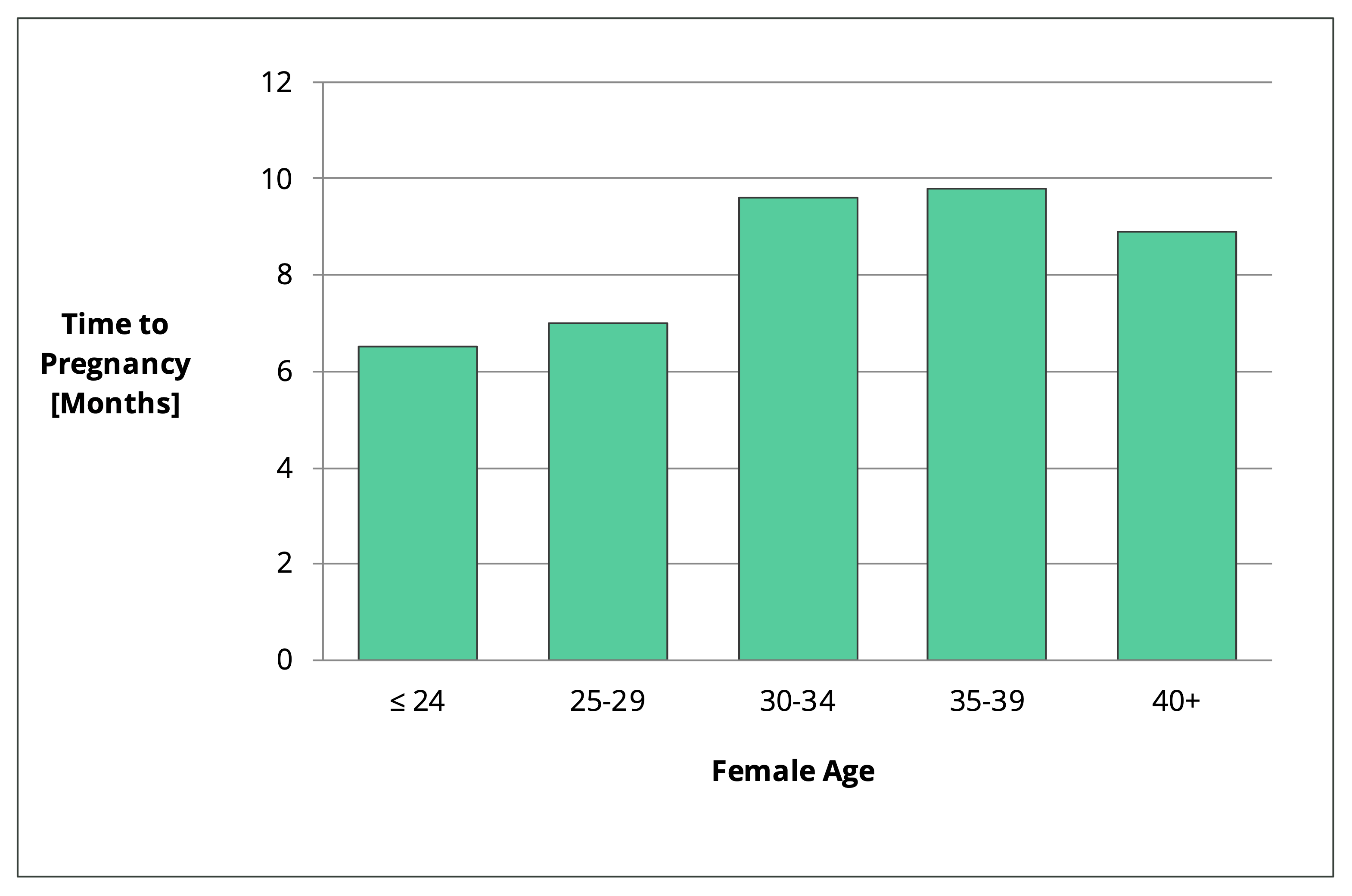
Figure 2. Time to pregnancy for couples trying to conceive their first child naturally [31].
Again, this data comes from a general population that is not specific to the wider PCOS population. This data set is only applicable to PCOS women that get their diagnosis under control. It can be assumed that women with unmanaged PCOS have much lower natural fertility. As mentioned above, 70-80% of women with unmanaged PCOS experience infertility [1, 2].
How to Increase Your Chances
I often get asked, “can you get pregnant with PCOS without taking medication?” Based on the previous section, the answer is clearly yes. But your chances are going to be much higher if you approach this project with intention. In my article How to Get Pregnant with PCOS, I describe the following evidence-based interventions:
- Follow a PCOS Diet
- Consider supplements
- Exercise regularly
- Manage your stress
- Track your cycle
- Get medical help when needed
Whether you’re trying to conceive naturally or you plan to get medical help, diet and lifestyle changes increase your odds of success. The key to a successful pregnancy is to get your PCOS under control first.
This is certainly the approach that Jamie took. After taking part in my free 30-Day PCOS Diet Challenge, Jamie went on to lose 50 lbs (23 kg). It took a complete overhaul of her diet and lifestyle to achieve such great results. But her drive to overcome four years of infertility spurred her on to her greatest joy.
You can read Jamie’s PCOS success story here.
When Do You Need Medical Help?
Most women with PCOS don’t need medical help to get pregnant. What they need are evidence-based diet and lifestyle changes. But, for women in their late 30s and beyond, it can make sense to seek medical help. There’s no denying that natural fertility declines at this age (see Figure 1). Seeking medical help is even more important if your partner has fertility issues too.
As I explain in my article How to Get Pregnant with PCOS, the use of metformin or birth control is a poor choice for improving fertility [27, 32-34]. Letrozole appears to be better than clomid for inducing ovulation [35-39]. But the combination of letrozole and clomid together may be better than using letrozole alone [40]. Gonadotropins are the big guns for ovulation induction. These products are typically used during intrauterine insemination (IUI) or in-vitro fertilization (IVF). Once you’re heading down the path of IVF you’re maximizing your chances of getting pregnant. This is an expensive procedure with several known hazards, but the success rates are the highest.
IVF treatment provides the best chances of getting pregnant with PCOS. This is also an area where women with PCOS may actually hold an advantage. Your chances of getting pregnant with PCOS don’t increase with age, but they don’t get worse. Unlike women without PCOS. The idea here is that PCOS women have higher ovarian reserve than age-matched controls. Because of this, PCOS women can produce more embryos during IVF. More embryos mean more transfer cycles, which leads to better cumulative birth rates [41, 42].
One of the consequences of this phenomenon is that age is less of a factor for PCOS women. A 2011 study on IVF patients with PCOS found that birth rates held stable between 22 and 41 years of age [43]. A similar study found that peak fertility was maintained until 38 years of age [44]. Others have found that PCOS women over 40 years have comparable success rates to those aged 35 to 40 [45].
The Bottom Line
Women with PCOS can definitely get pregnant but they face more obstacles. Unmanaged PCOS makes it harder to fall pregnant and carry a pregnancy to term.
But PCOS is a treatable condition that can be managed with diet and lifestyle changes. For women that adopt a PCOS diet, their chances of getting pregnant with PCOS naturally can be as good as non-PCOS women. Seeking medical help can make sense in some circumstances too. Male factor infertility and age should be the primary considerations here, rather than PCOS.
The right diet and lifestyle changes improve your chances regardless of how you try to conceive. If you’re trying to conceive, or you plan to soon, then set yourself up for success. Join my free 30-Day PCOS Diet Challenge today.
FAQ
Can you get pregnant with endometriosis and PCOS? Endometriosis adds a layer of complexity to an already complex PCOS diagnosis. But endometriosis is also a chronic inflammatory disorder. Because of this, PCOS natural treatments like diet and exercise should also ease the symptoms of this disorder.
Can you get pregnant with PCOS and fibroids? Dysregulation of inflammation and immune processes are involved in the formation of uterine fibroids [46, 47]. But unlike PCOS, fibroids don’t interfere with ovulation. They can make implantation more difficult and increase the chances of pregnancy loss though. A good specialist can develop a treatment plan to manage fibroids before or during pregnancy.
Can you get pregnant with PCOS and thyroid problems? Thyroid dysfunction presents an added obstacle to a healthy PCOS pregnancy. Untreated thyroid conditions reduce fertility and are linked to many pregnancy risks that are similar to PCOS. Find out how to get your thyroid checked properly here. The good news is that a PCOS-friendly diet is also good for thyroid dysfunction.
Can you get pregnant without ovulating with PCOS? No. If you don’t ovulate, you can’t get pregnant.
Can metformin help you get pregnant with PCOS? The Endocrine Society Clinical Practice Guidelines state that “[metformin] has limited or no benefit in treating infertility [33].” I explain why in my article Metformin for PCOS.
Can losing weight with PCOS help you get pregnant? Yes. Excess body fat has negative effects on egg quality, embryo development, and the receptivity of your uterus [18, 48]. For overweight women, losing weight is one of the best ways to improve fertility and pregnancy outcomes [49]. Weight loss of 5-10% can make a significant difference [50-53]. I explain how to lose weight with PCOS here.
Can you get pregnant with untreated PCOS? Yes. Some women get lucky. Untreated PCOS can reduce the quality of your pregnancy though, including the health outcomes for your children. Women with untreated PCOS are also more likely to experience poor health after giving birth.
How long after a miscarriage can you get pregnant with PCOS? After an early miscarriage (<6 weeks gestation), you should be fine to continue trying to conceive the following month. It may be better to wait a few months though after a later miscarriage. This will give your body a chance to restore a healthy nutrient status.
Can you get pregnant at 40 with PCOS without medication? Absolutely. But you must get your PCOS in check first.
Author
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.
References
1Melo, A.S., R.A. Ferriani, and P.A. Navarro, Treatment of infertility in women with polycystic ovary syndrome: approach to clinical practice. Clinics (Sao Paulo), 2015. 70(11): p. 765-9.
2Joham, A.E., et al., Prevalence of infertility and use of fertility treatment in women with polycystic ovary syndrome: data from a large community-based cohort study. J Womens Health (Larchmt), 2015. 24(4): p. 299-307.
3Barrea, L., et al., Source and amount of carbohydrate in the diet and inflammation in women with polycystic ovary syndrome. Nutr Res Rev, 2018. 31(2): p. 291-301.
4Carvalho, L.M.L., et al., Polycystic Ovary Syndrome as a systemic disease with multiple molecular pathways: a narrative review. Endocr Regul, 2018. 52(4): p. 208-221.
5González, F., Inflammation in Polycystic Ovary Syndrome: underpinning of insulin resistance and ovarian dysfunction. Steroids, 2012. 77(4): p. 300-5.
6González, F., et al., Hyperandrogenism sensitizes mononuclear cells to promote glucose-induced inflammation in lean reproductive-age women. Am J Physiol Endocrinol Metab, 2012. 302(3): p. E297-306.
7Popovic, M., G. Sartorius, and M. Christ-Crain, Chronic low-grade inflammation in polycystic ovary syndrome: is there a (patho)-physiological role for interleukin-1? Seminars in Immunopathology, 2019. 41(4): p. 447-459.
8Rudnicka, E., et al., Chronic Low Grade Inflammation in Pathogenesis of PCOS. Int J Mol Sci, 2021. 22(7).
9Wang, J., et al., Hyperandrogenemia and insulin resistance: The chief culprit of polycystic ovary syndrome. Life Sciences, 2019. 236.
10Sivasankari, R. and B. Usha, Reshaping the Gut Microbiota Through Lifestyle Interventions in Women with PCOS: A Review. Indian J Microbiol, 2022. 62(3): p. 351-363.
11Tremellen, K. and K. Pearce, Dysbiosis of Gut Microbiota (DOGMA)–a novel theory for the development of Polycystic Ovarian Syndrome. Med Hypotheses, 2012. 79(1): p. 104-12.
12He, F.F. and Y.M. Li, Role of gut microbiota in the development of insulin resistance and the mechanism underlying polycystic ovary syndrome: a review. J Ovarian Res, 2020. 13(1): p. 73.
13Patil, K., et al., Compromised Cumulus-Oocyte Complex Matrix Organization and Expansion in Women with PCOS. Reprod Sci, 2021.
14Chang, R.J. and H. Cook-Andersen, Disordered follicle development. Mol Cell Endocrinol, 2013. 373(1-2): p. 51-60.
15Palomba, S., J. Daolio, and G.B. La Sala, Oocyte Competence in Women with Polycystic Ovary Syndrome. Trends Endocrinol Metab, 2017. 28(3): p. 186-198.
16Patel, S.S. and B.R. Carr, Oocyte quality in adult polycystic ovary syndrome. Semin Reprod Med, 2008. 26(2): p. 196-203.
17Gonzalez, M.B., et al., Inflammatory markers in human follicular fluid correlate with lipid levels and Body Mass Index. J Reprod Immunol, 2018. 130: p. 25-29.
18Broughton, D.E. and K.H. Moley, Obesity and female infertility: potential mediators of obesity’s impact. Fertil Steril, 2017. 107(4): p. 840-847.
19Giudice, L.C., Endometrium in PCOS: Implantation and predisposition to endocrine CA. Best Pract Res Clin Endocrinol Metab, 2006. 20(2): p. 235-44.
20Schulte, M.M., J.H. Tsai, and K.H. Moley, Obesity and PCOS: the effect of metabolic derangements on endometrial receptivity at the time of implantation. Reprod Sci, 2015. 22(1): p. 6-14.
21Abdulkhalikova, D., et al., The Lifestyle Modifications and Endometrial Proteome Changes of Women With Polycystic Ovary Syndrome and Obesity. Front Endocrinol (Lausanne), 2022. 13: p. 888460.
22Sha, T., et al., A meta-analysis of pregnancy-related outcomes and complications in women with polycystic ovary syndrome undergoing IVF. Reprod Biomed Online, 2019. 39(2): p. 281-293.
23Matorras, R., et al., Polycystic ovarian syndrome and miscarriage in IVF: systematic revision of the literature and meta-analysis. Arch Gynecol Obstet, 2022.
24Luo, L., et al., Early miscarriage rate in lean polycystic ovary syndrome women after euploid embryo transfer – a matched-pair study. Reprod Biomed Online, 2017. 35(5): p. 576-582.
25Hart, R., PCOS and infertility. Panminerva Med, 2008. 50(4): p. 305-14.
26Lim, S.S., et al., Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database Syst Rev, 2019. 3(3): p. Cd007506.
27Legro, R.S., et al., Randomized Controlled Trial of Preconception Interventions in Infertile Women With Polycystic Ovary Syndrome. J Clin Endocrinol Metab, 2015. 100(11): p. 4048-58.
28Shang, Y., et al., Dietary Modification for Reproductive Health in Women With Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne), 2021. 12: p. 735954.
29Garruti, G., R. Depalo, and M. De Angelis, Weighing the Impact of Diet and Lifestyle on Female Reproductive Function. Curr Med Chem, 2019. 26(19): p. 3584-3592.
30Wesselink, A.K., et al., Age and fecundability in a North American preconception cohort study. Am J Obstet Gynecol, 2017. 217(6): p. 667.e1-667.e8.
31Konishi, S., et al., Fecundability and Sterility by Age: Estimates Using Time to Pregnancy Data of Japanese Couples Trying to Conceive Their First Child with and without Fertility Treatment. Int J Environ Res Public Health, 2021. 18(10).
32Sharpe, A., et al., Metformin for ovulation induction (excluding gonadotrophins) in women with polycystic ovary syndrome. Cochrane Database Syst Rev, 2019. 12(12): p. Cd013505.
33Legro, R.S., et al., Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab, 2013. 98(12): p. 4565-92.
34Legro, R.S., et al., Benefit of Delayed Fertility Therapy With Preconception Weight Loss Over Immediate Therapy in Obese Women With PCOS. J Clin Endocrinol Metab, 2016. 101(7): p. 2658-66.
35Amer, S.A., et al., Double-blind randomized controlled trial of letrozole versus clomiphene citrate in subfertile women with polycystic ovarian syndrome. Hum Reprod, 2017. 32(8): p. 1631-1638.
36Franik, S., et al., Aromatase inhibitors (letrozole) for subfertile women with polycystic ovary syndrome. Cochrane Database Syst Rev, 2018. 5(5): p. Cd010287.
37Franik, S., et al., Aromatase inhibitors for subfertile women with polycystic ovary syndrome. Cochrane Database Syst Rev, 2014(2): p. Cd010287.
38Wang, R., et al., First-line ovulation induction for polycystic ovary syndrome: an individual participant data meta-analysis. Hum Reprod Update, 2019. 25(6): p. 717-732.
39Yland, J.J., et al., Emulating a target trial of the comparative effectiveness of clomiphene citrate and letrozole for ovulation induction. Hum Reprod, 2022. 37(4): p. 793-805.
40Mejia, R.B., et al., A randomized controlled trial of combination letrozole and clomiphene citrate or letrozole alone for ovulation induction in women with polycystic ovary syndrome. Fertil Steril, 2019. 111(3): p. 571-578.e1.
41Mai, Z., et al., Comparison of Cumulative Live Birth Rate Between Aged PCOS Women and Controls in IVF/ICSI Cycles. Front Endocrinol (Lausanne), 2021. 12: p. 724333.
42Tannus, S., et al., Prevalence, clinical characteristics, and reproductive outcomes of polycystic ovary syndrome in older women referred for tertiary fertility care. Arch Gynecol Obstet, 2018. 297(4): p. 1037-1042.
43Mellembakken, J.R., et al., Sustained fertility from 22 to 41 years of age in women with polycystic ovarian syndrome. Hum Reprod, 2011. 26(9): p. 2499-504.
44Hwang, Y.I., et al., Fertility of patients with polycystic ovary syndrome undergoing in vitro fertilization by age. Int J Gynaecol Obstet, 2016. 135(1): p. 91-5.
45Li, J., et al., A Slower Age-Related Decline in Treatment Outcomes After the First Ovarian Stimulation for in vitro Fertilization in Women With Polycystic Ovary Syndrome. Front Endocrinol (Lausanne), 2019. 10: p. 834.
46Orciani, M., et al., Chronic Inflammation May Enhance Leiomyoma Development by the Involvement of Progenitor Cells. Stem Cells Int, 2018. 2018: p. 1716246.
47El Andaloussi, A., et al., Uterine Fibroids: Bridging Genomic Defects and Chronic Inflammation. Semin Reprod Med, 2017. 35(6): p. 494-498.
48Snider, A.P. and J.R. Wood, Obesity induces ovarian inflammation and reduces oocyte quality. Reproduction, 2019. 158(3): p. R79-r90.
49Cena, H., L. Chiovato, and R.E. Nappi, Obesity, Polycystic Ovary Syndrome, and Infertility: A New Avenue for GLP-1 Receptor Agonists. J Clin Endocrinol Metab, 2020. 105(8): p. e2695-709.
50Thomson, R.L., et al., The effect of a hypocaloric diet with and without exercise training on body composition, cardiometabolic risk profile, and reproductive function in overweight and obese women with polycystic ovary syndrome. J Clin Endocrinol Metab, 2008. 93(9): p. 3373-80.
51Stamets, K., et al., A randomized trial of the effects of two types of short-term hypocaloric diets on weight loss in women with polycystic ovary syndrome. Fertil Steril, 2004. 81(3): p. 630-7.
52Tolino, A., et al., Evaluation of ovarian functionality after a dietary treatment in obese women with polycystic ovary syndrome. Eur J Obstet Gynecol Reprod Biol, 2005. 119(1): p. 87-93.
53Kuchenbecker, W.K., et al., In women with polycystic ovary syndrome and obesity, loss of intra-abdominal fat is associated with resumption of ovulation. Hum Reprod, 2011. 26(9): p. 2505-12.
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.