If you’re interested in intermittent fasting and PCOS then it’s likely you have three key questions.
Will it help? How do I do it? What are the hazards? This article takes an evidence-based approach to answer these questions.
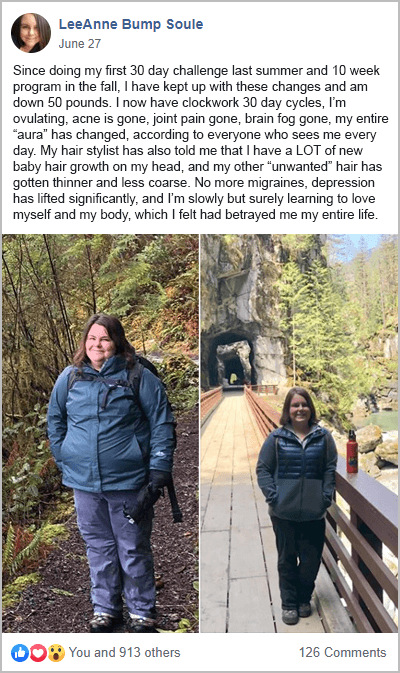
There’s disagreement on many aspects of fasting for PCOS. What’s not debatable though is that a healthy diet is essential. For many women who complete my free 30-Day PCOS Diet Challenge, a PCOS diet is enough for success.
See a worked example of a PCOS diet by downloading this free 3-Day Meal Plan.
Types of Intermittent Fasting
There are many ways to fast intermittently.
- Alternate day fasting.
- The 5:2 diet with two fast days and five feast days per week.
- Time-restricted eating.
Time-restricted eating is a fasting approach where you limit your “eating hours” each day. Essentially this just means either having an early dinner or a late breakfast. This is what most people mean when they talk about intermittent fasting for PCOS. So, that’s what we’ll focus on here. When I say, “intermittent fasting”, I mean time-restricted eating.
Is Intermittent Fasting Good for PCOS?
The most robust answer to this question is, “probably”. There’s a lot of good research on the health benefits of intermittent fasting. But few studies explore fasting interventions specifically in women with PCOS [1].
Fasting appears to alter insulin sensitivity which can have many positive effects on PCOS [2]. Bodyweight, fertility, acne, unwanted hair, and more are all improved with better insulin regulation. Studies in mice models of PCOS show that intermittent fasting improves metabolic and hormone profiles [3]. But that’s about as far as the trials go.
The most compelling evidence supporting intermittent fasting for PCOS comes from non-PCOS-specific studies. Here are three of the most salient findings.
1. Intermittent Fasting is Good for Metabolic Health
Intermittent fasting for metabolic syndrome is well-studied. Metabolic abnormalities are a common problem for many women with PCOS. The close link between PCOS and metabolic syndrome is why we have elevated risks for type 2 diabetes and cardiovascular disease.
Intermittent fasting is likely to be helpful if you have high blood pressure or insulin resistance. Researchers have seen good results across a range of metabolic biomarkers when restricting eating to a 4-10-hour window [4-7].
A 2020 meta-analysis found that time-restricted eating is, “a promising therapeutic strategy for controlling weight and improving metabolic dysfunctions…”
There is also supportive epidemiological data and a mechanistic understanding of fasting [8-11]. For example, fasting appears to support a robust circadian rhythm. It can also lead to an inadvertent reduction in caloric intake [7].
The short answer here is that if you have high blood pressure or insulin resistance, then intermittent fasting is worth trying. This is likely to include most PCOS women that are overweight. Your PCOS diagnosis doesn’t need to come into it. The decision should be made based on your metabolic health.
2. Intermittent Fasting is Good for Fertility
Insulin resistance is an underlying driver of PCOS infertility [12-16]. And intermittent fasting improves insulin sensitivity. Given these facts, it’s not hard to draw a link between intermittent fasting and improved fertility in women with PCOS.
But we can now go a step further with this view.
Intermittent fasting may have anti-aging effects. The mechanisms are complicated, but this idea seems robust [17]. In 2023, researchers found that intermittent fasting reversed the effects of egg quality declining with age [18]. This trial was a rodent study. But if the results hold up in people too, this will be big news if you’re trying to conceive.
3. Intermittent Fasting May Help Prevent Breast Cancer
There’s a big overlap between the metabolic risk factors of PCOS and other diseases. Breast cancer is one of the more controversial of these diseases [19-22]. Whether there’s a causal link or not, intermittent fasting may lower your breast cancer risks.
This is because diet, weight gain, and obesity may be responsible for up to 50% of breast cancer cases [23-26]. Disruptions of circadian rhythms may also be associated with abnormal cell division and tumor growth [27]. Intermittent fasting addresses both of these problems. This is why some public health researchers now recommend fasting as part of a healthy lifestyle [28].
How to Start Intermittent Fasting for PCOS
If you’re going to try time-restricted eating, here are five steps to follow.
1. Follow a PCOS Diet
The most important first step is to embrace a PCOS diet. That’s what my free 30-Day PCOS Diet Challenge is all about. What you eat is much more important than when you eat. Many women learn to manage their PCOS by dietary change alone.
Intermittent fasting should be seen as a tool for further improving a PCOS diet. As a stand-alone treatment, it’s unlikely to yield life-changing results.
For example, intermittent fasting in the absence of other interventions doesn’t help with weight loss [29].
2. Start Slowly
When it comes to shortening your eating window, I recommend starting easy. Aim to keep your food consumption to within 12 hours each day. This can be a challenge at first, so don’t be surprised if it’s harder than you expect.
Once you find that 12 hours of fasting feels easy, slowly increase your fasting period over several weeks. If you find that your hunger is overbearing near the end of your fast, you should dial things back to a more comfortable level. The same goes if you experience any other adverse effects. Your body needs time to adjust, so be kind to yourself. Feeling tired, cranky, or lightheaded are all signs you’re overdoing it. Pushing through could do more harm than good.
3. Be Careful When Fasting for Over 16 Hours
Limiting eating to 10-12 hours a day is likely to provide benefits. This is a good level of fasting for many women with PCOS.
That said, longer fasts may be better. This will depend on your individual circumstances.
I recommend caution when fasting for longer than 16 hours. The marginal health benefits beyond this duration are likely to be small. The potential for adverse effects is also likely to increase. More on this below.
4. Eat Early Rather Than Late
You have two choices when limiting your eating window. You can eat early and fast in the evening, or you can eat late and fast in the morning.
From a practical perspective, many people prefer to fast in the morning and eat at night. This means they can skip breakfast and can enjoy dinner at a normal hour. Based on the evidence to date though, eating early and fasting at night appears to be better [9, 30].
5. Check-In with Your Health Care Provider
Many experts have different views on the suitability of intermittent fasting for PCOS. Especially over the long term. This is partly due to differences in the fasting regimes and patients used in various clinical trials [31, 32].
But the weight of evidence suggests that limiting food intake to 8-12 hours per day is safe for most people [33-37].
If you’re unsure, then discuss your fasting regime with your healthcare provider. This is especially important if you’re pregnant or taking medication.
Hazards of Intermittent Fasting with PCOS
There are several hazards to consider when intermittent fasting with PCOS.
1. Disordered Eating
The most important is how it affects your relationship with food. Many participants in my free 30-Day PCOS Diet Challenge come to the program having years of failed dieting. Disordered eating is also a huge problem within our community [38].
For these women, forming a healthier relationship with food is mission-critical. Intermittent fasting has the potential to become a new diet obsession that interferes with this process. Research suggests that fasting doesn’t increase disordered eating behavior [39]. But caution is still warranted. If fasting feels like another diet, then it may not be right for you.
Time-restricted eating has been shown to improve quality of life [40]. If that’s not the case, then take this as a warning sign.
2. Hypoglycemia
Special care is needed when intermittent fasting while taking certain medications. For example, fasting can increase hypoglycemic events when taking metformin [41]. Because of the insulin-sensitizing effects of fasting, dosages may need to be reduced.
3. Hormone Imbalances
Many people on the internet claim that fasting can disrupt female hormone balance. Scientific support for these claims tends to be limited. The majority of studies cited have been conducted on animals rather than humans. They also use more intense fasting regimes beyond modest time-restricted eating [42, 43].
Doctor Helen Kollias, provides a balanced assessment of intermittent fasting here. Kollias describes the mechanisms by which fasting is different in women than men. That’s super-important. But she also calls out PCOS, as a specific situation where fasting may be beneficial.
The Bottom Line
There aren’t many studies that specifically look at intermittent fasting for PCOS. But there’s a lot of research showing that time-restricted eating is good for metabolic health. It may improve fertility, and also lower breast cancer risks. These factors are all very relevant to women with PCOS.
Intermittent fasting may not be suitable for women with disordered eating habits. Beyond this issue though, modest fasting is likely to be a safe intervention. For the best results, it’s essential to follow a PCOS-friendly diet. Without changing what you eat, changing the timing of your meals is likely to have limited benefits.
FAQ
TLDR: What’s the best intermittent fasting for PCOS? Research shows that eating early in the day, and fasting at night is likely to be the best approach to time-restricted eating [9, 30]. Start by shortening your eating window to 10-12 hours per day. If you want to fast for longer, be careful when going beyond 16 hours without food.
What about OMAD for PCOS? Having one meal a day (OMAD) is an intense form of intermittent fasting. The added cost/benefit of fasting for 23 hours compared to a more modest fast may not stack up for many women with PCOS. Caution is warranted as adverse effects are more likely with OMAD for PCOS.
What about lean PCOS and intermittent fasting? Is there a benefit? Lean PCOS women can have metabolic abnormalities just like women with a more classical type of PCOS. For these people, intermittent fasting is likely to be helpful. The other benefits also make intermittent fasting a helpful intervention for lean women with PCOS.
What about alternate day fasting for PCOS? Alternate-day fasting is when you reduce your caloric intake to around 500 calories every other day. This type of fasting is also being studied as a PCOS treatment [2]. A recent analysis found that alternate day fasting was better for weight loss than time-restricted eating [44]. But better studies are needed before solid conclusions can be made. Compliance challenges may make alternate day fasting more difficult for some people.
Intermittent fasting PCOS fertility. Can it help? This largely comes down to your metabolic health. For women with PCOS, improving metabolic health is a powerful way to overcome PCOS infertility. For PCOS women with metabolic abnormalities, intermittent fasting could help improve fertility.
Author
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.
References
1Floyd, R., et al., The Effect of Time-Restricted Eating on Insulin Levels and Insulin Sensitivity in Patients with Polycystic Ovarian Syndrome: A Systematic Review. Int J Endocrinol, 2022. 2022: p. 2830545.
2Chiofalo, B., et al., Fasting as possible complementary approach for polycystic ovary syndrome: Hope or hype? Med Hypotheses, 2017. 105: p. 1-3.
3Han, Y., et al., Time-restricted feeding improves metabolic and endocrine profiles in mice with polycystic ovary syndrome. Front Endocrinol (Lausanne), 2022. 13: p. 1057376.
4Wilkinson, M.J., et al., Ten-Hour Time-Restricted Eating Reduces Weight, Blood Pressure, and Atherogenic Lipids in Patients with Metabolic Syndrome. Cell Metab, 2020. 31(1): p. 92-104.e5.
5Cienfuegos, S., et al., Time restricted eating for the prevention of type 2 diabetes. J Physiol, 2022. 600(5): p. 1253-1264.
6Cienfuegos, S., et al., Effects of 4- and 6-h Time-Restricted Feeding on Weight and Cardiometabolic Health: A Randomized Controlled Trial in Adults with Obesity. Cell Metab, 2020. 32(3): p. 366-378.e3.
7Jamshed, H., et al., Effectiveness of Early Time-Restricted Eating for Weight Loss, Fat Loss, and Cardiometabolic Health in Adults With Obesity: A Randomized Clinical Trial. JAMA Intern Med, 2022. 182(9): p. 953-962.
8Chaix, A., et al., Time-Restricted Eating to Prevent and Manage Chronic Metabolic Diseases. Annu Rev Nutr, 2019. 39: p. 291-315.
9Duan, D., et al., Time-Restricted Eating in Metabolic Syndrome-Focus on Blood Pressure Outcomes. Curr Hypertens Rep, 2022. 24(11): p. 485-497.
10Li, M.D., Clock-modulated checkpoints in time-restricted eating. Trends Mol Med, 2022. 28(1): p. 25-35.
11Manoogian, E.N.C., et al., Time-restricted Eating for the Prevention and Management of Metabolic Diseases. Endocr Rev, 2022. 43(2): p. 405-436.
12Barrea, L., et al., Source and amount of carbohydrate in the diet and inflammation in women with polycystic ovary syndrome. Nutr Res Rev, 2018. 31(2): p. 291-301.
13Cena, H., L. Chiovato, and R.E. Nappi, Obesity, Polycystic Ovary Syndrome, and Infertility: A New Avenue for GLP-1 Receptor Agonists. J Clin Endocrinol Metab, 2020. 105(8): p. e2695-709.
14Fica, S., et al., Insulin resistance and fertility in polycystic ovary syndrome. J Med Life, 2008. 1(4): p. 415-22.
15Morley, L.C., et al., Insulin-sensitising drugs (metformin, rosiglitazone, pioglitazone, D-chiro-inositol) for women with polycystic ovary syndrome, oligo amenorrhoea and subfertility. Cochrane Database Syst Rev, 2017. 11(11): p. Cd003053.
16Wang, J., et al., Hyperandrogenemia and insulin resistance: The chief culprit of polycystic ovary syndrome. Life Sciences, 2019. 236.
17Jamshed, H., et al., Early Time-Restricted Feeding Improves 24-Hour Glucose Levels and Affects Markers of the Circadian Clock, Aging, and Autophagy in Humans. Nutrients, 2019. 11(6).
18Li, C., et al., Intermittent fasting reverses the declining quality of aged oocytes. Free Radic Biol Med, 2023. 195: p. 74-88.
19Barry, J.A., M.M. Azizia, and P.J. Hardiman, Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update, 2014. 20(5): p. 748-58.
20Carvalho, M.J., et al., Controversial association between polycystic ovary syndrome and breast cancer. Eur J Obstet Gynecol Reprod Biol, 2019. 243: p. 125-132.
21Wang, C., et al., Mendelian randomization analyses for PCOS: evidence, opportunities, and challenges. Trends Genet, 2022. 38(5): p. 468-482.
22Zhu, T. and M.O. Goodarzi, Causes and Consequences of Polycystic Ovary Syndrome: Insights From Mendelian Randomization. J Clin Endocrinol Metab, 2022. 107(3): p. e899-e911.
23Bissell, M.C.S., et al., Breast Cancer Population Attributable Risk Proportions Associated with Body Mass Index and Breast Density by Race/Ethnicity and Menopausal Status. Cancer Epidemiol Biomarkers Prev, 2020. 29(10): p. 2048-2056.
24Blot, W.J. and R.E. Tarone, Doll and Peto’s quantitative estimates of cancer risks: holding generally true for 35 years. J Natl Cancer Inst, 2015. 107(4).
25Sprague, B.L., et al., Proportion of invasive breast cancer attributable to risk factors modifiable after menopause. Am J Epidemiol, 2008. 168(4): p. 404-11.
26Wilson, L.F., et al., Population attributable risk of modifiable risk factors associated with invasive breast cancer in women aged 45-69 years in Queensland, Australia. Maturitas, 2013. 76(4): p. 370-6.
27Wegrzyn, L.R., et al., Rotating Night-Shift Work and the Risk of Breast Cancer in the Nurses’ Health Studies. Am J Epidemiol, 2017. 186(5): p. 532-540.
28Christensen, R.A.G. and A.A. Kirkham, Time-Restricted Eating: A Novel and Simple Dietary Intervention for Primary and Secondary Prevention of Breast Cancer and Cardiovascular Disease. Nutrients, 2021. 13(10).
29Lowe, D.A., et al., Effects of Time-Restricted Eating on Weight Loss and Other Metabolic Parameters in Women and Men With Overweight and Obesity: The TREAT Randomized Clinical Trial. JAMA Intern Med, 2020. 180(11): p. 1491-1499.
30Cienfuegos, S., et al., Effect of Intermittent Fasting on Reproductive Hormone Levels in Females and Males: A Review of Human Trials. Nutrients, 2022. 14(11).
31Petersen, M.C., et al., Complex physiology and clinical implications of time-restricted eating. Physiol Rev, 2022. 102(4): p. 1991-2034.
32Schuppelius, B., et al., Time Restricted Eating: A Dietary Strategy to Prevent and Treat Metabolic Disturbances. Front Endocrinol (Lausanne), 2021. 12: p. 683140.
33Gabel, K., et al., Time-Restricted Eating to Improve Cardiovascular Health. Curr Atheroscler Rep, 2021. 23(5): p. 22.
34Moon, S., et al., Beneficial Effects of Time-Restricted Eating on Metabolic Diseases: A Systemic Review and Meta-Analysis. Nutrients, 2020. 12(5).
35Moro, T., et al., Twelve Months of Time-restricted Eating and Resistance Training Improves Inflammatory Markers and Cardiometabolic Risk Factors. Med Sci Sports Exerc, 2021. 53(12): p. 2577-2585.
36Uldal, S., et al., Is Time-Restricted Eating Safe in the Treatment of Type 2 Diabetes?-A Review of Intervention Studies. Nutrients, 2022. 14(11).
37Anic, K., et al., Intermittent Fasting-Short- and Long-Term Quality of Life, Fatigue, and Safety in Healthy Volunteers: A Prospective, Clinical Trial. Nutrients, 2022. 14(19).
38Lee, I., et al., Increased risk of disordered eating in polycystic ovary syndrome. Fertil Steril, 2017. 107(3): p. 796-802.
39Varady, K.A., et al., Cardiometabolic Benefits of Intermittent Fasting. Annu Rev Nutr, 2021. 41: p. 333-361.
40Crose, A., et al., Time-Restricted Eating Improves Quality of Life Measures in Overweight Humans. Nutrients, 2021. 13(5).
41Corley, B.T., et al., Intermittent fasting in Type 2 diabetes mellitus and the risk of hypoglycaemia: a randomized controlled trial. Diabet Med, 2018. 35(5): p. 588-594.
42Alexander, B.M., et al., Influence of short-term fasting during the luteal phase of the estrous cycle on ovarian follicular development during the ensuing proestrus of ewes. Anim Reprod Sci, 2007. 97(3-4): p. 356-63.
43Kumar, S. and G. Kaur, Intermittent fasting dietary restriction regimen negatively influences reproduction in young rats: a study of hypothalamo-hypophysial-gonadal axis. PLoS One, 2013. 8(1): p. e52416.
44Elortegui Pascual, P., et al., A meta-analysis comparing the effectiveness of alternate day fasting, the 5:2 diet, and time-restricted eating for weight loss. Obesity (Silver Spring), 2022.
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.